What can you expect during a fast? How exactly does fasting work? Can you eat during a fast? Here we take a look at how the body changes during fasting. Then we discuss how to prepare for a fast.
Below you can find:
- What Happens During Fasting?
- What Is the Timeline of Changes During Fasting?
- Where Does Each Fasting Method Lie on the Fasting Timeline?
- What Interrupts the Fasting Timeline?
- What Can You Eat While Fasting Without Losing the Benefits?
- Summary: The Takeaways
- Continuing the Series on Fasting
Below you will learn the timeline of fasting and how to prepare for a fast.
Check out the Summary Takeaways section at the end to see how to plan for a fast. Then come back and grab all the details and references to go over with your doctor. That way you’ll be fully prepared and get the most from your fast.
What Happens During Fasting?
At its core, “fasting” describes different methods of calorie restriction. Calorie restriction is the research term for reduced food intake.
Fasting methods differ in how much, how long, and how often they restrict calories.
The calories you normally eat come from carbohydrates, fats, and proteins. When you fast, you deprive your body of these fuels. This forces your body to pull from its fuel reserves.
During fasting:
-
Carbohydrates come from glycogen, the body’s storage form of carbohydrate
-
Fats come from your body fat stores
-
Amino acids mainly come from the proteins in your muscle
As you’ll see below, glycogen is used first as your body adapts to using fat as your main fuel source. Then protein is consumed to maintain your blood glucose levels.
Should You Worry About Muscle Loss During Fasting?
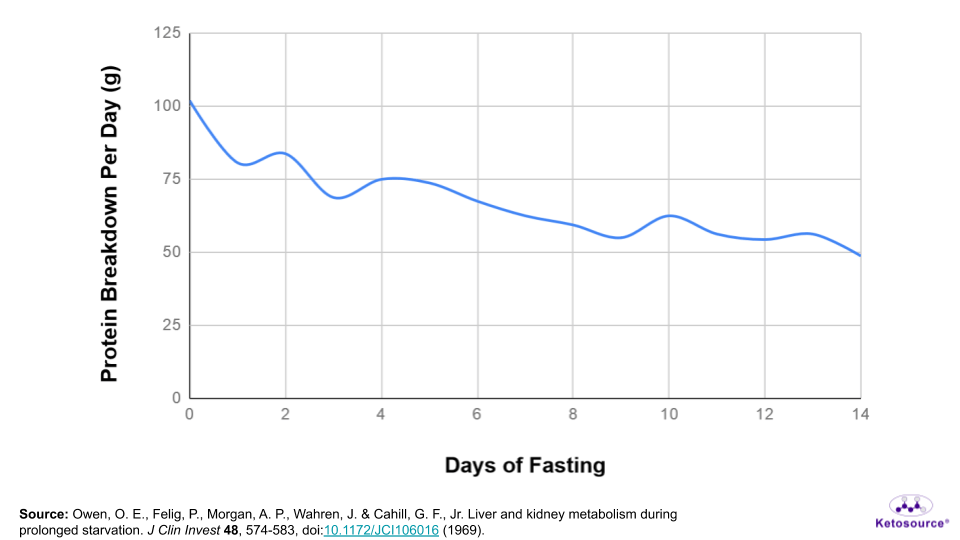
Many people worry about losing muscle during fasting. It is true that you lose some protein during a fast, and your muscle is the main source of this protein.
But the amount of protein you consume during a fast is surprisingly small. You’ll lose an estimated 1.1-1.2 lbs of protein during a 7-day fast.
To put this into perspective, people can lose 5 lbs or more during a week of fasting. This means only ~20% of weight loss comes from protein if you fast for a week.
Your body taps into these fuel reserves as hormone levels begin changing. Hormones are chemical messengers that carry signals throughout the body.
Insulin, glucagon, insulin-like growth factor 1 (IGF1), and growth hormone are some of the major hormones affected by fasting. These hormones are described in more detail later.
These hormones control large-scale changes during fasting, like what you see in the mirror. They also control small-scale changes, like what happens at the cellular level in your body.
What Is the Timeline of Changes During Fasting?
Studies on prolonged fasting paint the clearest picture of the fasting timeline.
Your hormones and metabolism change considerably within just one week of fasting.
A week of fasting may seem like an eternity without food. When you compare it to a normal 15-hour eating window, i.e. eating from 7 AM to 10 PM, an entire week of fasting can seem like a very long time.
But people have been studied during fasts lasting much longer than one week. In general, the first week of fasting establishes the major changes to hormones and metabolism that continue during longer fasts.
Falling Back onto Fuel Reserves
During fasting, your body’s liver glycogen is tapped first. Glycogen is a storage form of carbohydrate which consists of long, branched strings of glucose.
Your largest glycogen stores are found in your liver and muscle cells. But during fasting, only your liver’s glycogen is used to control your blood glucose level. This is because your muscle cells can’t make the enzyme glucose-6-phosphatase. This enzyme is necessary to release glucose into the bloodstream.
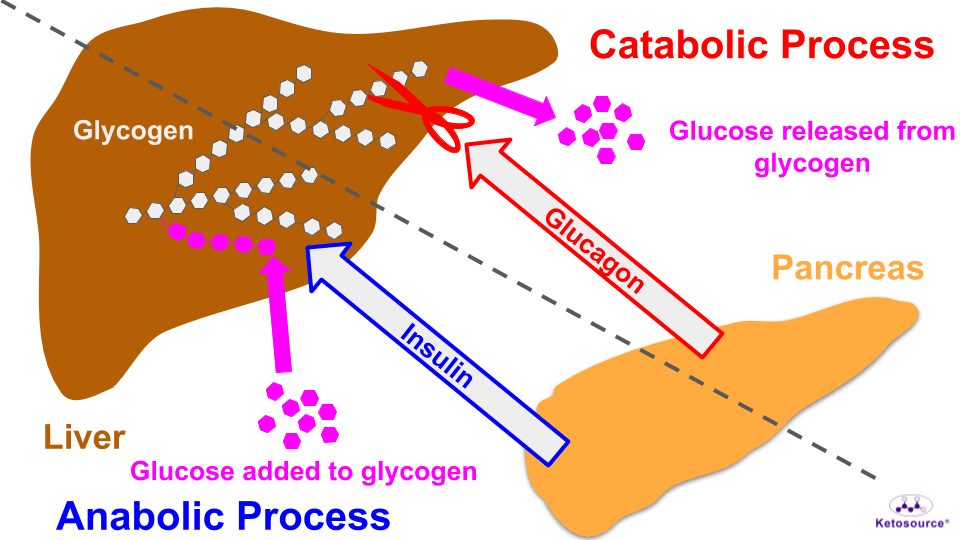
Another organ, your pancreas, controls how liver glycogen is used during fasting.
Your Pancreas Controls Your Carbohydrate Reserves
When you eat carbohydrates like bread or rice, they are converted into glucose and this increases your blood glucose level. When your blood glucose level rises, your pancreas secretes the hormone insulin into your bloodstream.
Insulin shuttles excess glucose out of your blood and into cells throughout your body. These cells can then use the glucose or store it as glycogen. In this way your liver and muscle are basically large glucose “sinks”, as liver cells and muscle cells can store lots of glycogen.
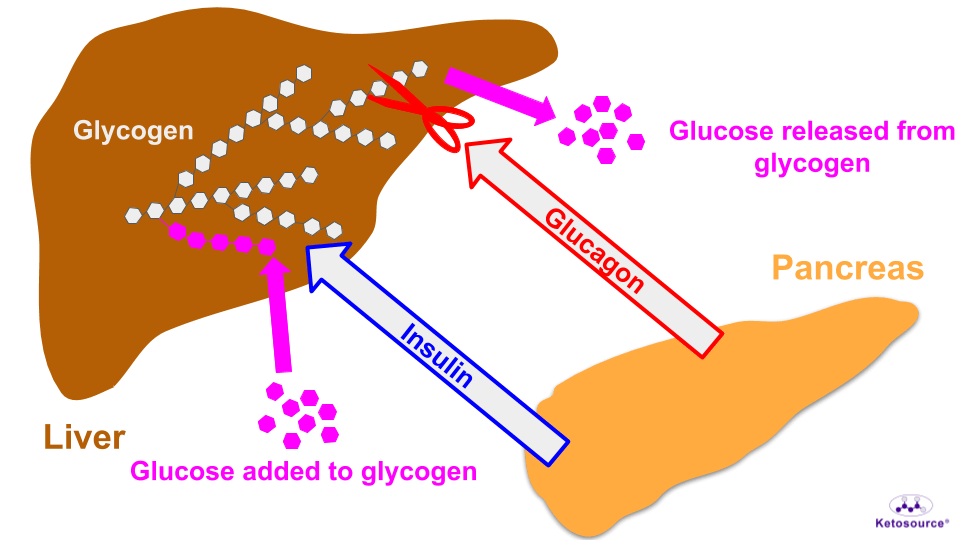
When you stop eating carbohydrates, your pancreas secretes glucagon into your bloodstream. Glucagon stimulates your liver cells to break down glycogen and this raises your blood glucose levels. You can see this illustrated in Figure 1 below.
Figure 1. The effect of insulin and glucagon on liver glycogen.
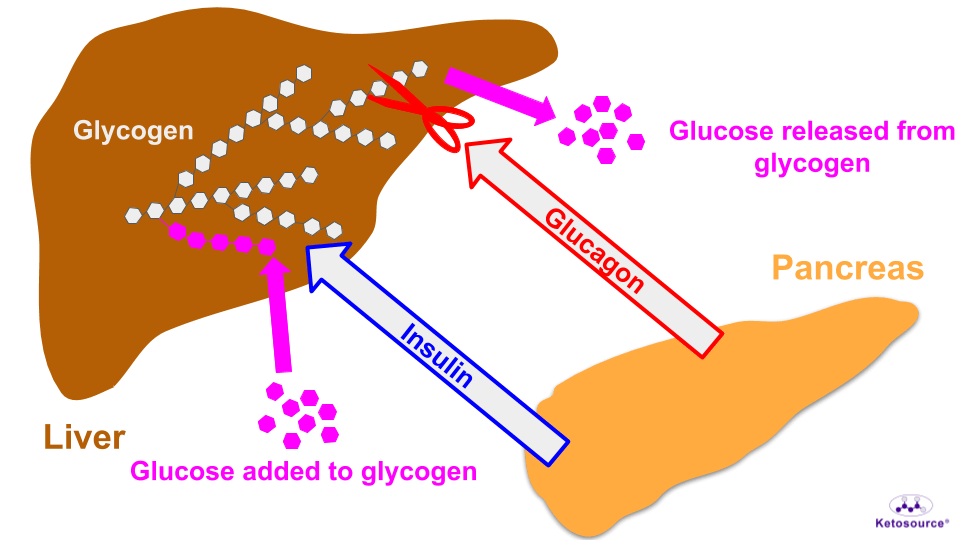
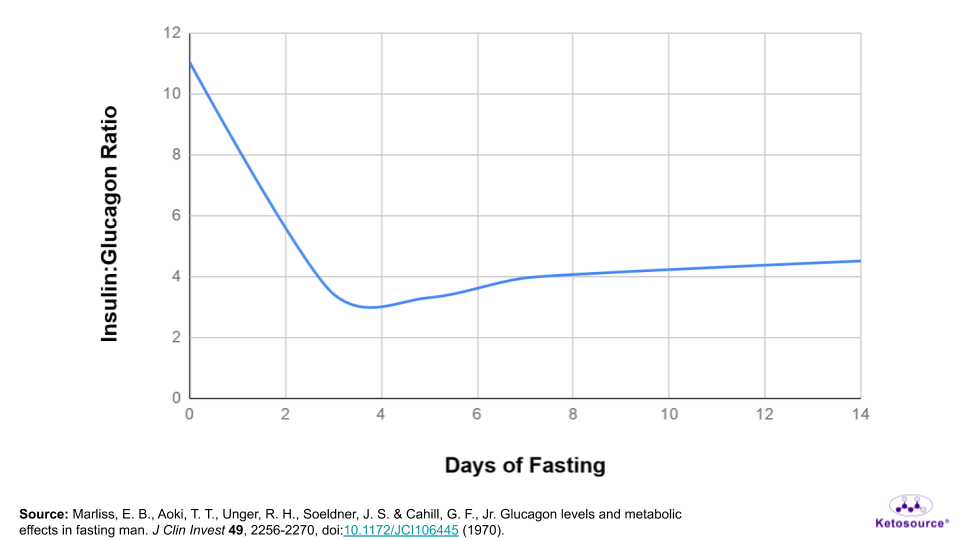
Altogether, the hormones insulin and glucagon both come from your pancreas and play “tug-of-war” on your liver glycogen. The ratio of insulin to glucagon will determine who wins. This ratio tells you whether glucose is going into or coming out of the liver.
During a normal day of eating, this overall process helps to keep your blood glucose levels at a certain set point. Unless you’ve eaten within the last few hours, your blood glucose is probably ~5 mM (~90 mg/dL) right now.
It works like a thermostat. When your blood glucose rises, insulin comes out and brings it back down again. When your blood glucose falls, glucagon comes out to bring it back up again.
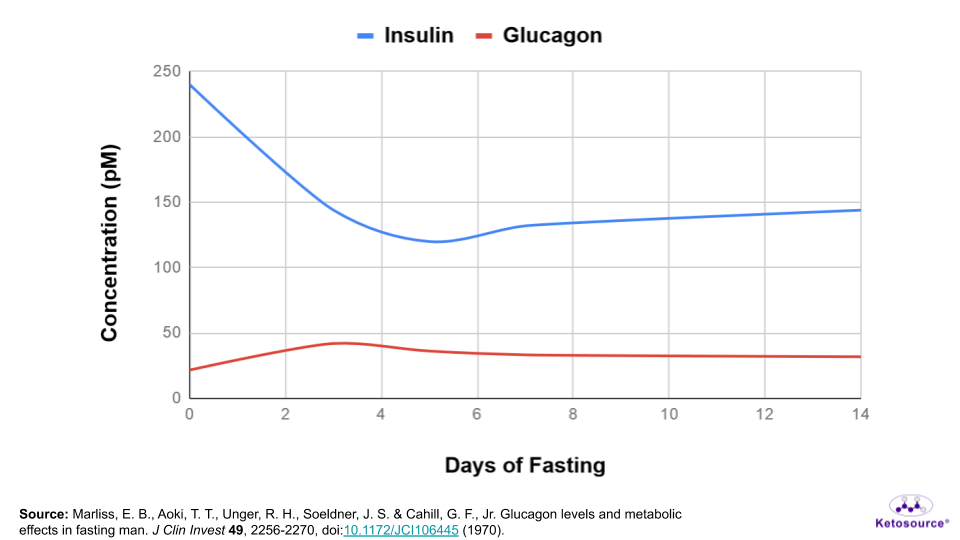
During fasting, insulin levels progressively drop as glucagon levels rise. This means glucagon wins the tug-of-war on liver glycogen. You can see this in Figures 2 and 3 below.
Figure 2. The levels of insulin and glucagon during fasting.
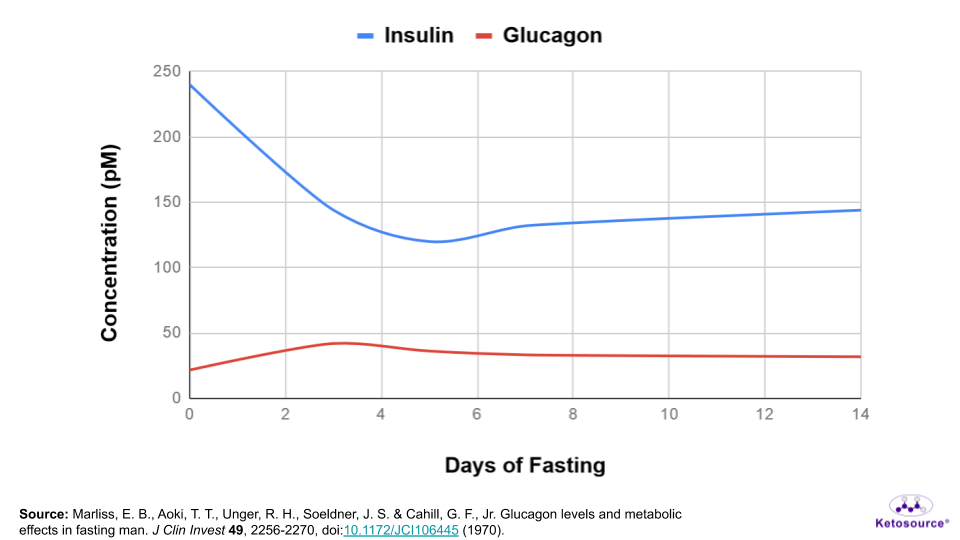
Figure 3. The insulin:glucagon ratio during fasting.
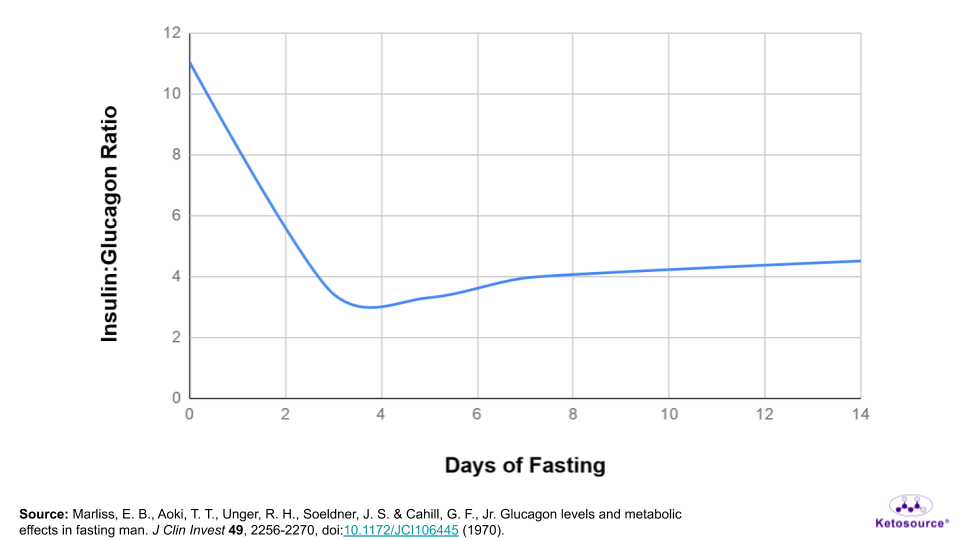
Your liver holds an estimated 70 grams of glycogen. This tug-of-war on liver glycogen allows it to last 2-4 days during prolonged fasting.
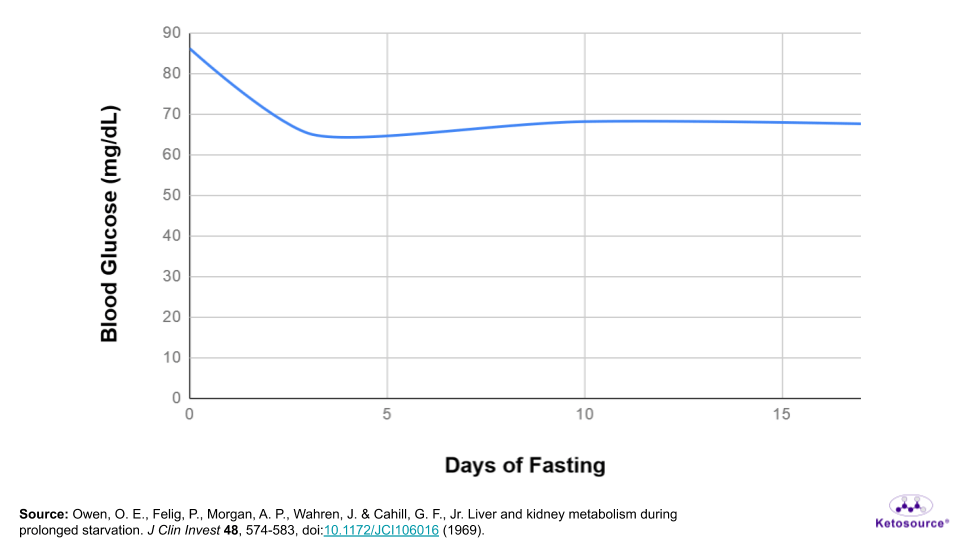
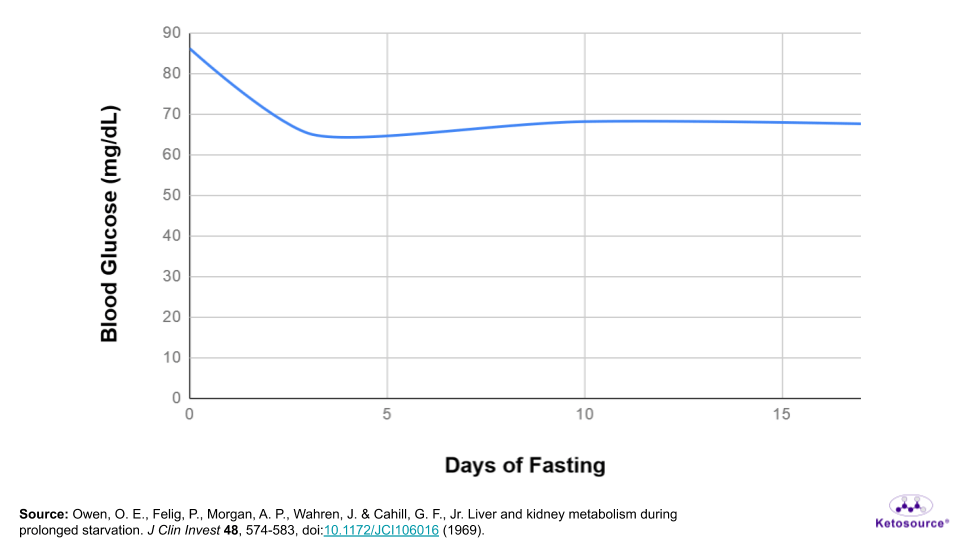
As you can see in Figure 4 below, blood glucose levels drop to a new set point below 70 mg/dL during this time.
Figure 4. Blood glucose levels drop during fasting.
What About Hypoglycemia?
Hypoglycemia has very uncomfortable and potentially dangerous symptoms. The mild symptoms of hypoglycemia include nervousness, sweating, and increased heart rate and blood pressure.
Surprisingly, non-diabetic people who are fasting are protected against the symptoms of hypoglycemia. The high levels of ketone bodies in their blood are believed to be responsible for this. Ketone bodies are the breakdown products, or metabolites, of fat.
Should You Worry About Hypoglycemia During Fasting?
Studies found that non-diabetic people who fasted for >6 weeks did not show symptoms of hypoglycemia, even at incredibly low blood glucose levels. But this does not mean it’s impossible to become hypoglycemic during fasting.
Certain medical conditions such as insulinoma and glycogen storage diseases can cause hypoglycemia during fasting. Type 2 diabetics who take blood glucose-lowering medications are also at risk for hypoglycemia during fasting, even if they eat food on their fasting days.
Type 1 diabetics are at risk for both hypoglycemia and hyperglycemia during fasting. Because of this volatility in blood glucose levels, there is not enough research yet to recommend any fasting method for type 1 diabetics.
Fasting Puts You into Ketosis
The buildup of ketone bodies in the blood is called ketosis. In fact, the ketogenic diet was developed to mimic fasting since they both put you in ketosis.
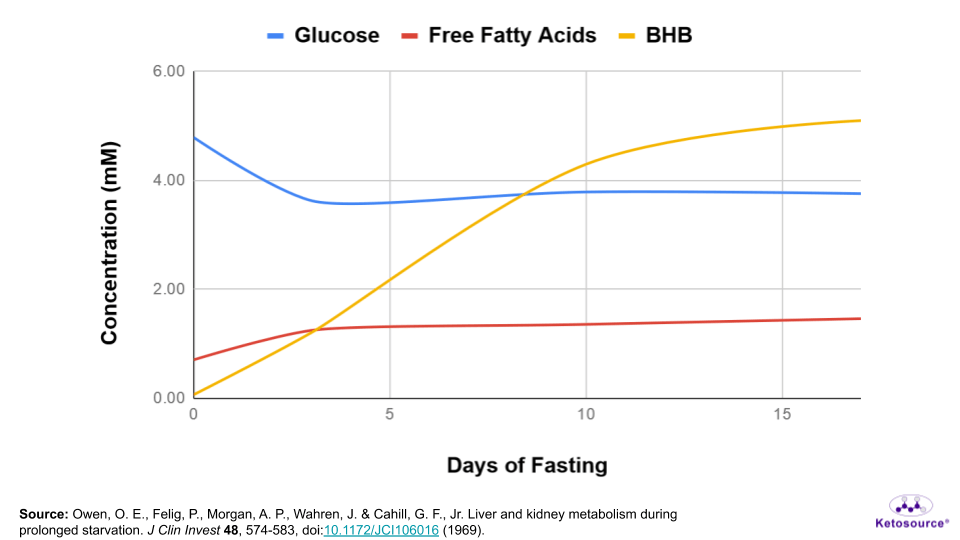
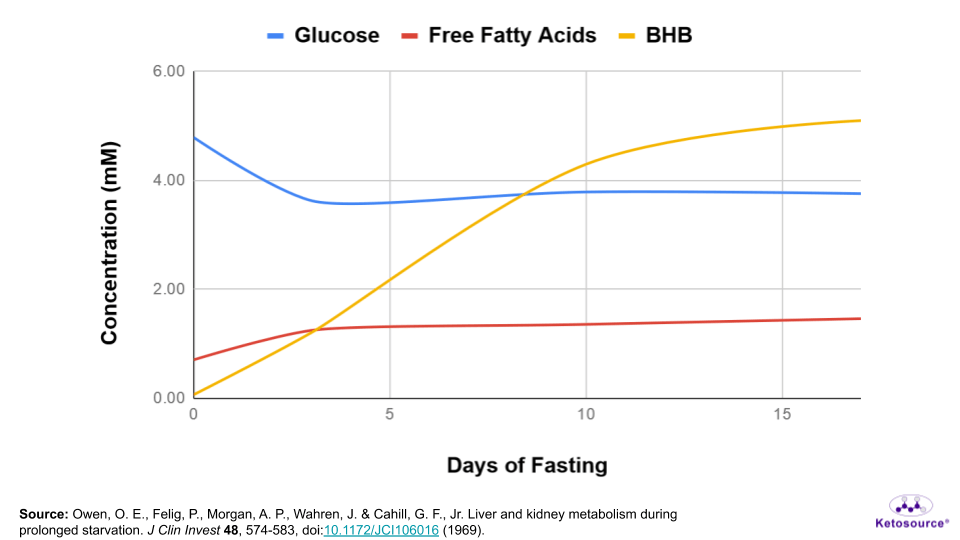
As you run out of liver glycogen, your body taps into its fat reserves and begins creating ketone bodies. Blood levels of free fatty acids and ketone bodies increase during fasting.
Use a Ketogenic Diet to Make Fasting Easier
Following a ketogenic diet for at least 4 weeks may help with fasting. One reason for this is because your body adapts to using less glucose within 4 weeks on the ketogenic diet.
You can see in Figure 5 below that as blood glucose falls, levels of free fatty acids and beta-hydroxybutyrate rise in the blood. Beta-hydroxybutyrate is the predominant ketone body your body makes while fasting.
Figure 5. How blood levels of glucose, free fatty acids, and beta-hydroxybutyrate (BHB) change during fasting.
Your blood glucose set point drops during fasting, but it does not drop to zero. This means new glucose needs to be made during fasting.
New glucose is generated during fasting through a process called gluconeogenesis. Just like the name gluco-neo-genesis implies, new (neo) glucose (gluco) is generated (genesis) during fasting. As noted earlier, some gluconeogenesis comes from the amino acids of protein during fasting.
Some gluconeogenesis also comes from glycerol during fasting. Glycerol is the backbone of triglycerides, which is your body’s main storage form of fat. Triglycerides get broken down into fatty acids and glycerol. The fatty acids can then be converted into ketone bodies and the glycerol can be converted into glucose.
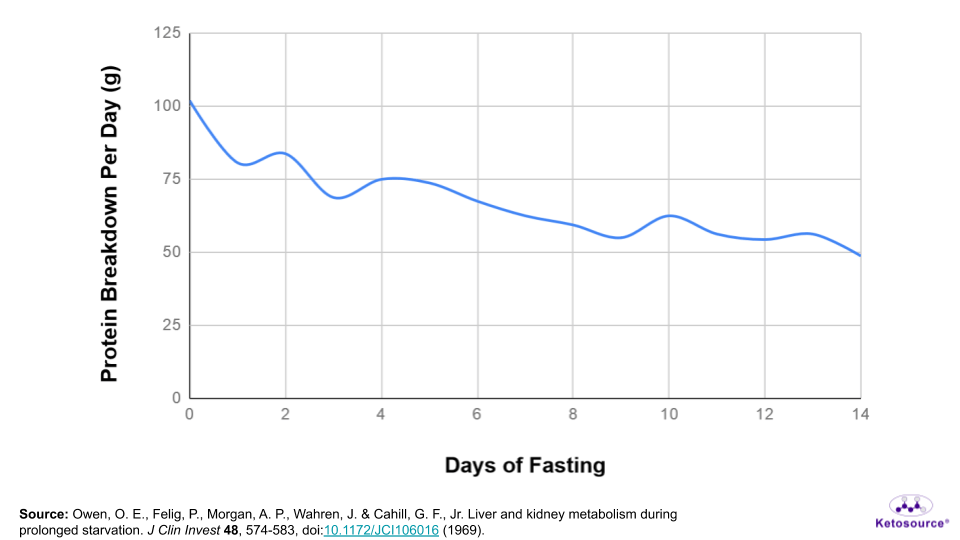
So, some muscle protein does get broken down during fasting. As mentioned earlier, total protein breakdown amounts to only ~1.1-1.2 lbs during a 7-day fast. This means it is not a major concern during fasting. You can see a timeline of protein breakdown in Figure 6 below.
Figure 6. The estimated breakdown of protein per day during fasting.
To help put things into perspective, an obese person may carry ~750,000 calories of fat but only ~30,000 calories of protein on their body. If they relied heavily on protein for fuel during fasting, they could not safely fast for very long. But obese individuals like this have safely fasted for several months. One obese man even fasted for 382 days!
In summary, fat becomes the primary fuel source for the body during the first week of water-only fasting. Afterwards, the size of the fat reserves determines how long a person can safely fast before breaking down too much muscle.
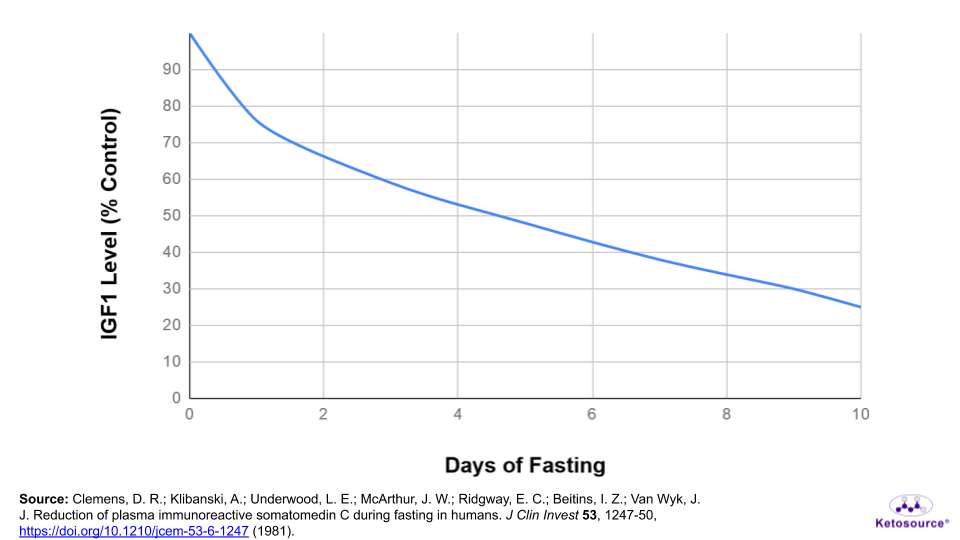
The Growth Hormone/IGF1 Axis
Growth hormone and IGF1 are two hormones which control the growth of the body. You may have heard of them before in the context of childhood growth or muscle growth.
Growth hormone is normally released during the night while you sleep, though it can also be released during the day.
Growth hormone signals your liver to produce IGF1. IGF1 then triggers pro-growth mechanisms throughout your body. This is called the growth hormone/IGF1 axis.
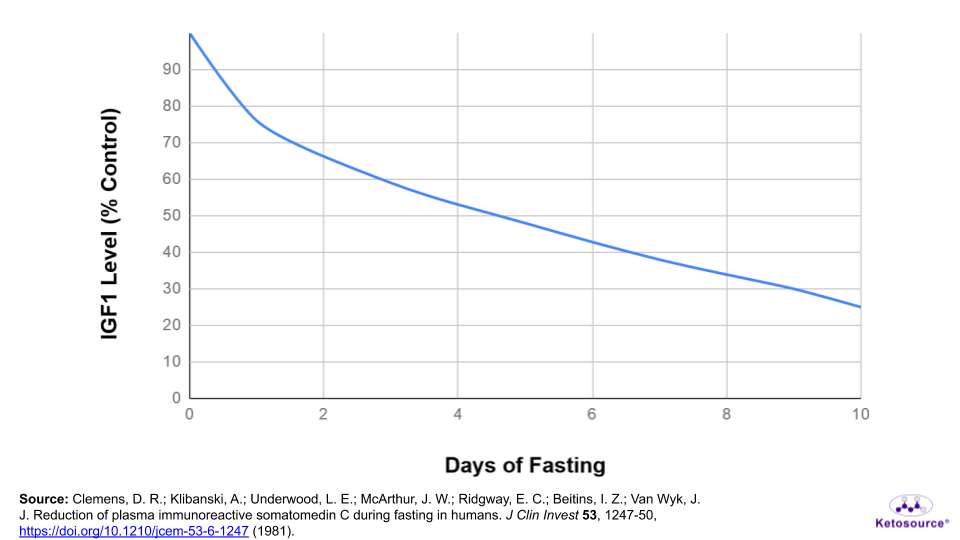
During fasting, the growth hormone/IGF1 axis becomes muted. Growth hormone levels peak more often during fasting and the total growth hormone release is higher than normal. But instead of increasing like growth hormone, IGF1 levels drop during fasting.
Figure 7. How IGF1 levels change during fasting.
This observation for growth hormone seems rather strange considering its pro-growth effects. You probably don’t think about “growth” being an important part of fasting. Why would growth hormone stay elevated when a person is fasting?
Growth hormone helps regulate fuel use during fasting. High levels of growth hormone are necessary to increase fat breakdown during fasting. Growth hormone also promotes the liver to release more glucose into the bloodstream. This helps deplete the liver glycogen reserve more quickly as the body shifts to fat metabolism.
So, growth hormone goes up during fasting and this promotes a switch to fat metabolism. This surprisingly does not increase IGF1 levels, which instead drop during a prolonged fast.
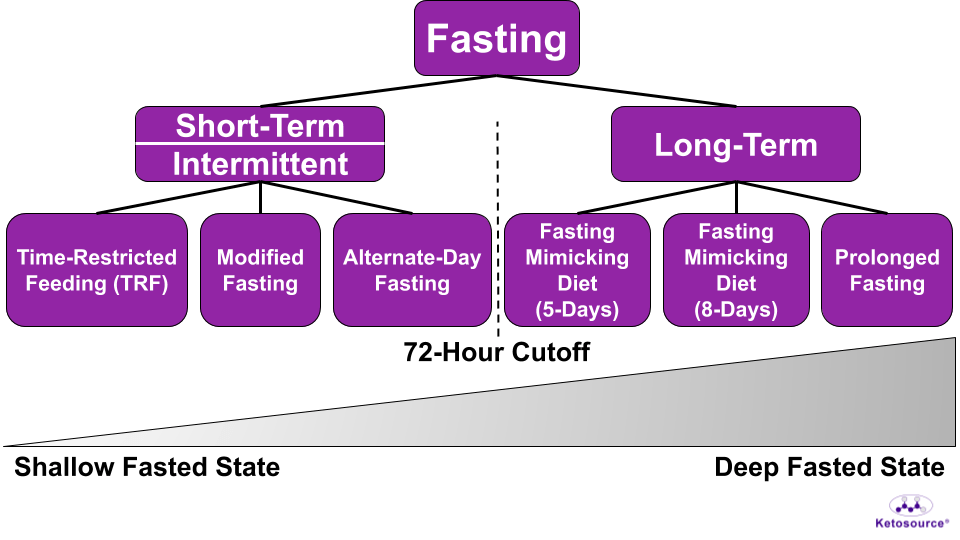
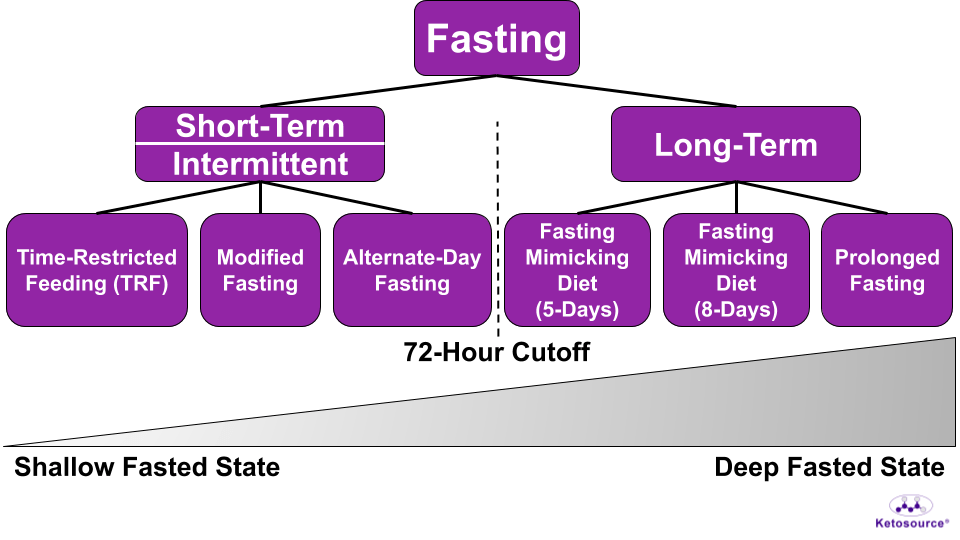
Where Does Each Fasting Method Lie on the Fasting Timeline?
The fasting timeline in the graphs above outlines the key changes in hormones and metabolism which take place during fasting. Each of the fasting methods will come with at least some of these changes.
To get an idea of how the fasting timeline relates to each fasting method, you can imagine two different states of the body when it comes to food:
-
Anabolism is the building up of complex structures like glycogen and muscle protein. When your body is in an anabolic state, it is building these structures.
-
Catabolism is the breaking down of these complex structures. When your body is in a catabolic state, it is breaking down structures like glycogen and muscle protein.
The effect of insulin and glucagon on glycogen illustrates this well. Figure 8 shows this below.
Figure 8. Anabolism and catabolism control the size of glycogen in the liver.
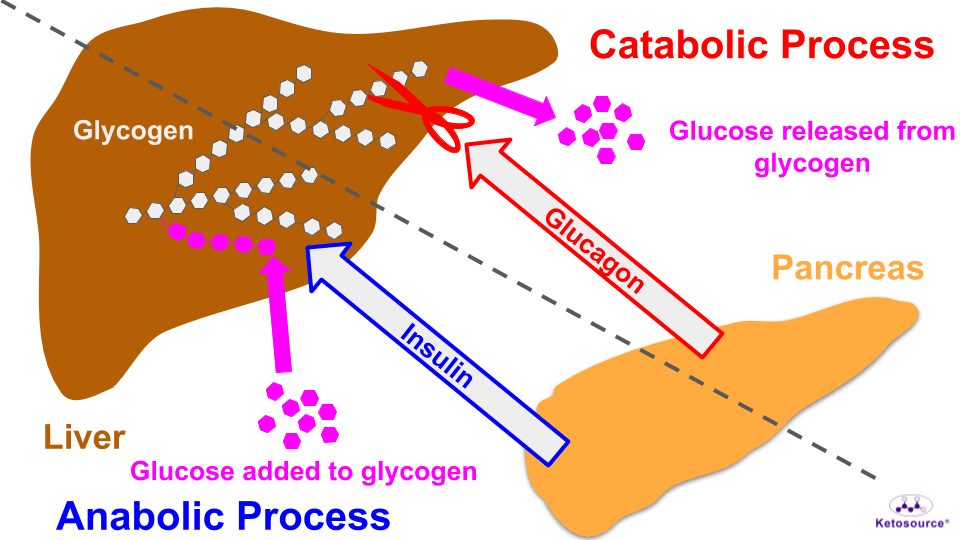
Fasting promotes catabolism. This means fasting puts you into an overall catabolic state where complex structures are broken down.
Since fasting promotes catabolism, the catabolic state will be called the Fasted State from now on. The anabolic state will be called the Fed State.
Each fasting method has its place. The fasting method which is best for you will depend on a couple of factors:
-
How deep of a Fasted State do you need?
-
Do you need to take food/medication to make sure your fast is safe and successful?
The Fed and Fasted States
Among the hormones discussed in the fasting timeline above, insulin and IGF1 are hormones of the Fed State. Insulin stimulates the buildup of glycogen and muscle protein. IGF1 stimulates the buildup of muscle protein.
These hormones of the Fed State decrease during prolonged fasting.
On the other hand, glucagon and growth hormone are hormones of the Fasted State. Glucagon stimulates the breakdown of glycogen and the formation of ketone bodies. Growth hormone stimulates the breakdown of glycogen and triglycerides.
These hormones of the Fasted State increase during prolonged fasting.
You can think of a Fasted State as a “rest period” from food and growth.
Type 2 diabetes is a great example of this. Entering a rest period from food is helping treat and potentially “reverse” type 2 diabetes. Entering a rest period periodically may even prevent diseases like type 2 diabetes.
Also, studies on stem cells suggest that a rest period can allow old cells to die off while stem cells expand in number. Then entering a Fed State after this rest period allows the body to make use of the new stem cells.
Studies like these are discussed in the “Fasting Goals” sections below. As you’ll see, the depth of your Fasted State will depend on your fasting goal.
Measuring Your Fasted State
It is not simple to track hormone changes during a fast. But the Fasted State comes with a drop in blood glucose levels and a rise in blood ketone body levels. Glucose and ketone bodies are easy to measure using an over-the-counter blood meter.
This means you can gauge your Fasted State by tracking these blood measurements.
Which Fasting Methods Have the Deepest Fasted States?
The depth of your Fasted State depends on how much you restrict calories and for how long you restrict calories.
You can think of this as a spectrum.
On one end of the spectrum is time-restricted feeding (TRF). The fasting window is short (<24 hours) and there is no calorie restriction. So TRF has the shallowest Fasted State.
On the opposite end of the spectrum is prolonged fasting. The fasting window is long (≥72 hours) and calories are completely restricted. So prolonged fasting has the deepest Fasted State.
The other fasting methods fall somewhere in the middle.
For modified fasting, the number of days you choose to restrict calories will determine the net calorie deficit for the week.
On a weekly timeline, alternate-day fasting and modified fasting can both result in calorie deficits. This is certainly true of alternate-day fasting, which fully restricts calories on up to four days of the week.
So, between these two methods, alternate-day fasting has a deeper Fasted State than modified fasting. Placing the 5-day Fasting Mimicking Diet (FMD) and 8-day FMD on the spectrum is a little more difficult.
(NOTE: Fasting Mimicking Diet, FMD, and Prolon are registered trademarks of L-Nutra)
The 5-day FMD and 8-day FMD both involve prolonged calorie restriction of ≤50% calories/day. This means they each have deeper Fasted States than modified fasting or alternate-day fasting. This must be true for the 8-day FMD as it has a lower calorie limit.
If you consider prolonged fasting as eight days of water-only fasting, then the spectrum of Fasted States looks like Figure 9 below.
Figure 9. The spectrum of Fasted States.
Do You Always Want the Deepest Fasted State?
So, because prolonged fasting has the deepest Fasted State, shouldn’t everyone just do that? What is the purpose of these other fasting methods?
Not necessarily. As discussed in the Fasting Goals section below, a deep Fasted State is useful some of the time. You don’t always want to stay there.
Also, some of the benefits of TRF relate to the circadian rhythm. The circadian rhythm is a daily variation in certain physiological markers like hormone levels. The idea here is that your eating habits are normally out of sync with your circadian rhythm, and TRF helps correct this.
This makes TRF the ideal starting place if you have never fasted before. You can get used to shallow Fasted State and get a more tuned circadian rhythm by following TRF.
This will also help you gain the confidence to try the methods with deeper Fasted States. Succeeding at one fasting method is better than giving up after failing at another fasting method.
Medications During Fasting
If you are on medication which requires food, then you’ll want to use a fasting method which lets you eat every day.
This is especially true if you are on a medication which lowers your blood glucose levels such as metformin, insulin, and sulfonylureas. Even with modified fasting, type 2 diabetics on these medications can get hypoglycemia.
The type of medication and the dose are important to consider when fasting. You should always discuss a strategy with your doctor before beginning any fasting method.
What Interrupts the Fasting Timeline?
In general, it is best to limit your food intake during your fasting window to no-calorie beverages.
This includes coffee, tea, saltwater/bouillon, and even flavored no-calorie beverages. In fact, you lose electrolytes during prolonged fasting, so replacing them periodically is a good idea. Salty water and magnesium supplements are good for replacing electrolytes.
Remember that insulin and IGF1 are hormones of the Fed State. The higher they go, the more they take you out of your Fasted State. That can interfere with your fasting goals.
What Affects IGF1 Levels?
Studies on fasting and calorie restriction suggest that IGF1 levels are increased mostly by protein and carbohydrates. Fat does not have as much impact on IGF1.
Overall calorie intake is important here as well, as a low-calorie intake will not stimulate IGF1 very much during fasting.
For example, after a 5-day fast, a healthy person at 150 lbs (68 kg) could eat 68 g protein and 750 calories total for three or four days without rebounding their IGF1 level.
Even the 5-day FMD, which allows for a similar amount of calories and much less protein, drops IGF1 levels by 24%.
So, what does this mean for your fast? This suggests that very low amounts of protein (<<68 g) and total calories (<<750 kcal) can be taken during your fasting window if necessary.
What Affects Insulin Levels?
Foods rich in protein and/or carbohydrates also stimulate insulin release. This means that eating foods rich in carbohydrates and/or protein during a fast will take you out of your Fasted State.
Fat has little effect on insulin. This means fat is a better choice than carbohydrates or protein when fasting.
Certain fibers do not impact blood glucose or insulin much either. In fact, high-fiber foods impact blood glucose and insulin less than their low-fiber counterparts.
What Can You Eat While Fasting Without Losing the Benefits?
You want to minimize foods which take you out of your Fasted State. This means you should minimize foods which increase your blood glucose, insulin, and IGF1.
Foods high in fat and fiber and low in protein and non-fiber carbohydrates (e.g. avocados) are ideal if you need to eat while fasting.
See How Food Affects Your Fasted State
If you have a blood glucose/ketone monitor, you can check on your Fasted State after eating something.
To do this, measure your blood glucose and ketone bodies before you eat the food item. Then measure again one hour after eating it.
If your glucose goes up and/or your ketone bodies go down, then the food item increases your insulin and should be avoided.
When in doubt, consider these questions:
-
How does the food item impact your blood glucose and insulin levels? Aim for foods high in fat and fiber and low in protein and non-fiber carbohydrates.
-
How much of each food item do you want to consume while fasting? In general, high-carbohydrate and/or high-protein foods will increase your insulin. If you eat enough of them, they will also increase your IGF1 levels.
Table 1 lists foods that people often want to take while fasting. It can help you answer the questions above when you want to eat something during fasting.
Table 1. What to expect from foods during fasting. References for each item are included where available.
| Category |
Item |
Blood Sugar Triggered? |
Insulin Triggered? |
| Supplements |
Vitamin C |
No |
No |
| Activated Charcoal |
No |
No |
| Multivitamin (Unsweetened) |
No |
No |
| Blackseed Oil |
No |
No |
| Magnesium Supplement |
No |
No |
| Collagen Supplement |
No |
Likely |
| Diatomaceous Earth |
No |
No |
| Exogenous Ketone Bodies |
MCT Oil |
No |
Slight |
| C8 MCT Oil |
No |
Slight |
| Ketone Salts |
No |
Slight |
| Ketone Esters |
No |
Slight |
| Drinks And Liquids |
Coffee (Black) |
No |
No |
| Tea (Plain) |
No |
No |
| Almond Milk (Unsweetened) |
Possibly |
Possibly |
| Milk |
Yes |
Yes |
| Bone Broth |
No |
Likely |
| Protein Shake |
No |
Yes |
| Kombucha |
Likely |
Likely |
| Kefir |
Yes |
Yes |
| Herbs/Spices/Sweeteners |
Erythritol |
No |
No |
| Stevia |
No |
No |
| Xylitol |
Slight |
Slight |
| Black Pepper |
No |
No |
Summary: The Takeaways
Takeaways: How To Prepare For Fasting
-
Follow a ketogenic diet for four weeks before fasting. This will get you fat-adapted and make fasting easier.
-
If you’ve never fasted before, follow TRF first to get a feel for it. This can be as simple as ending your last meal by 7 PM every day.
-
If you take medications that require food, plan to eat foods high in fat and fiber and low in protein and high-glycemic carbohydrates.
-
Use a glucose/ketone meter to check how foods affect you. This will help you pick out foods which can be safe for your fast if you need them.
Takeaways: Making Fasting Easier
-
If the hunger is overwhelming, eat a small amount of high-fat/high-fiber food to help get you through. This includes avocados and MCT oil.
-
Go for short walks to take your mind off the fast. Staying active will help ease the hunger until it passes.
Takeaways: Executing Your Fast
-
Sip on saltwater/bouillon during the day to keep your electrolytes up. Avoid too much coffee as it will make you lose electrolytes more quickly.
-
The re-feed after prolonged fasting is very important. Avoid high glycemic carbohydrates (e.g. fruit juices, candy, cereal, etc.) as you will be fat-adapted and not carb-adapted after a fast. Have a high-fiber shake as your first meal after the fast to prevent stomach issues.
-
For the prolonged fasting re-feed, introduce solid foods slowly after the high-fiber shake. Solid foods high in fat and protein will satisfy your hunger and help you avoid overeating. Overeating will feel very uncomfortable as it brings on stomach issues and hiccups. Gradually increase your solid food intake over a couple of days as you feel more comfortable with it.
Continuing the Series on Fasting
Click here to continue reading about fasting. In Fasting Part 2, you will learn which fasting method is best for each fasting goal.
References
{5748374:WX6XVYQC};{5748374:4NT5FZFW};{5748374:WX6XVYQC};{5748374:KLVNMBHR};{5748374:CXS8BFWR};{5748374:WX6XVYQC},{5748374:4TLPENTP};{5748374:4NT5FZFW};{5748374:MAVD78JV};{5748374:82WAU8AK};{5748374:9R8B7N39};{5748374:4TLPENTP};{5748374:4NT5FZFW};{5748374:I256XB9K};{5748374:4TLPENTP};{5748374:QWP452KJ};{5748374:QWP452KJ},{5748374:NSWUNWIW};{5748374:QWP452KJ};{5748374:XUCLT9S5};{5748374:DGDTQT9G};{5748374:U5V47653};{5748374:VMKSQVPV};{5748374:WX6XVYQC};{5748374:L7YCZNPB};{5748374:X9FNS82E};{5748374:WX6XVYQC};{5748374:WX6XVYQC};{5748374:WX6XVYQC};{5748374:4NT5FZFW};{5748374:G7V6SP9C};{5748374:X9FNS82E};{5748374:4NT5FZFW};{5748374:8D52CF3M};{5748374:KNTYW8DU};{5748374:8D52CF3M};{5748374:MTRD6RAM};{5748374:8D52CF3M};{5748374:E6IMUMCA};{5748374:2VX4FBZ4};{5748374:4TLPENTP},{5748374:E6IMUMCA};{5748374:4TLPENTP},{5748374:8D52CF3M};{5748374:FHKFCPN3};{5748374:C4WVT4WG};{5748374:SQU9ZGIQ};{5748374:3WVQ9RWW},{5748374:3HHU6VZN};{5748374:3HHU6VZN};{5748374:J7ZVR9HH};{5748374:8D52CF3M};{5748374:DGDTQT9G};{5748374:ABKJEBZH};{5748374:P2Z6B7GC};{5748374:CPKGMASN};{5748374:CPKGMASN};{5748374:QGSWE9C6};{5748374:QGSWE9C6};{5748374:3HHU6VZN};{5748374:L2TIML6J};{5748374:7YAEJB2G};{5748374:58VR3TRJ};{5748374:TZX9Q4YD};{5748374:YNG6EDMA};{5748374:K573CTYQ};{5748374:K573CTYQ};{5748374:P9KSH38T};{5748374:P9KSH38T};{5748374:P9KSH38T};{5748374:P9KSH38T};{5748374:VLZHFYQ6};{5748374:VLZHFYQ6};{5748374:K6DR3X9T};{5748374:K6DR3X9T};{5748374:5MKG75AP};{5748374:5MKG75AP};{5748374:SB2KG3MB};{5748374:SB2KG3MB};{5748374:MT8PEC4G};{5748374:MT8PEC4G}
3d-printed-materials-and-systems
default
asc
0
8444
%7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A950%2C%22request_next%22%3A50%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22PNNNMDCY%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Dietze%20et%20al.%22%2C%22parsedDate%22%3A%221976%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDietze%20G%2C%20Wicklmayr%20M%2C%20Grunst%20J%2C%20Mehnert%20H%20%281976%29%20%5BThe%20anti-ketogenic%20effect%20of%20fructose%5D.%20Verh%20Dtsch%20Ges%20Inn%20Med%2082%20Pt%201%3A767%26%23x2013%3B769%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22%5BThe%20anti-ketogenic%20effect%20of%20fructose%5D%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%22%2C%22lastName%22%3A%22Dietze%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Wicklmayr%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Grunst%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22H.%22%2C%22lastName%22%3A%22Mehnert%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221976%22%2C%22language%22%3A%22ger%22%2C%22DOI%22%3A%22%22%2C%22ISSN%22%3A%220070-4067%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%5D%2C%22dateModified%22%3A%222020-04-17T10%3A10%3A51Z%22%7D%7D%2C%7B%22key%22%3A%22UMT4FS8S%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lee%20and%20Wolever%22%2C%22parsedDate%22%3A%221998-12%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLee%20BM%2C%20Wolever%20TM%20%281998%29%20Effect%20of%20glucose%2C%20sucrose%20and%20fructose%20on%20plasma%20glucose%20and%20insulin%20responses%20in%20normal%20humans%3A%20comparison%20with%20white%20bread.%20Eur%20J%20Clin%20Nutr%2052%3A924%26%23x2013%3B928.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsj.ejcn.1600666%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsj.ejcn.1600666%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Effect%20of%20glucose%2C%20sucrose%20and%20fructose%20on%20plasma%20glucose%20and%20insulin%20responses%20in%20normal%20humans%3A%20comparison%20with%20white%20bread%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20M.%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%20M.%22%2C%22lastName%22%3A%22Wolever%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVE%3A%20To%20determine%20the%20plasma%20glucose%20and%20insulin%20responses%20of%20various%20doses%20of%20glucose%2C%20sucrose%2C%20fructose%20and%20white%20bread%20in%20normal%20human%20subjects.%5CnDESIGN%3A%20Plasma%20glucose%20and%20insulin%20were%20measured%20before%20and%20at%20various%20times%20after%208%20subjects%20ate%2013%20different%20test%20meals%20in%20randomized%20order%20on%20separate%20days%20after%20an%20overnight%20fast.%20Test%20meals%20consisted%20of%20500%20ml%20of%20tea%20or%20water%20to%20which%20was%20added%20either%20nothing%2C%2025%2C%2050%2C%20or%20100%20g%20of%20glucose%20or%20sucrose%2C%2025%20or%2050%20g%20fructose%2C%2050%20g%20glucose%20plus%2050%20g%20fructose%2C%20or%20a%2025%2C%2050%20or%20100%20g%20carbohydrate%20portion%20of%20white%20bread.%20The%20glycaemic%20%28GI%29%20and%20insulinaemic%20index%20%28II%29%20values%20of%20the%20sugars%20were%20calculated%20by%20expressing%20the%20incremental%20areas%20under%20the%20plasma%20glucose%20and%20insulin%20curves%20%28AUC%29%20after%20glucose%2C%20sucrose%20and%20fructose%20as%20a%20percentage%20of%20the%20respective%20AUC%20after%20white%20bread%20containing%20the%20same%20amount%20of%20carbohydrate.%5CnSETTING%3A%20University%20teaching%20hospital%20clinical%20nutrition%20centre.%5CnSUBJECTS%3A%20Lean%2C%20normal%20subjects%20%284%20male%2C%204%20female%29%2021-33%20y%20of%20age.%5CnRESULTS%3A%20Plasma%20insulin%20responses%20increased%20nearly%20linearly%20as%20carbohydrate%20intake%20increased%20from%200%20to%20100%20g%2C%20but%20glycaemic%20responses%20increased%20by%20only%2068%25%20and%2038%25%20as%20carbohydrate%20intake%20increased%20from%2025%20to%2050%20g%20and%2050%20to%20100g%2C%20respectively.%20The%20GI%20and%20II%20values%20of%20glucose%2C%20149%2B%5C%2F-16%20and%20147%2B%5C%2F-18%2C%20respectively%2C%20were%20significantly%20greater%20than%20those%20of%20bread%20%28100%3B%20P%26lt%3B0.05%29%2C%20while%20the%20values%20for%20fructose%2C%2016%2B%5C%2F-4%20and%2022%2B%5C%2F-3%20were%20significantly%20less%20than%20those%20of%20bread%20%28P%26lt%3B0.001%29.%20GI%20values%20did%20not%20differ%20significantly%20from%20II%20values.%5CnCONCLUSIONS%3A%20It%20is%20concluded%20that%2C%20in%20normal%20subjects%2C%20as%20carbohydrate%20intake%20is%20increased%20from%200%20to%20100%20g%2C%20plasma%20insulin%20responses%20increase%20at%20a%20greater%20rate%20than%20plasma%20glucose%20responses.%20The%20insulinaemic%20responses%20elicited%20by%20glucose%2C%20sucrose%20or%20fructose%20are%20similar%20to%20those%20that%20would%20be%20expected%20from%20a%20starchy%20food%20with%20the%20same%20glycaemic%20index.%22%2C%22date%22%3A%22Dec%201998%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1038%5C%2Fsj.ejcn.1600666%22%2C%22ISSN%22%3A%220954-3007%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%226ZD5MYAL%22%5D%2C%22dateModified%22%3A%222020-04-17T10%3A08%3A36Z%22%7D%7D%2C%7B%22key%22%3A%226X22CVSE%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHypometabolism%20as%20a%20therapeutic%20target%20in%20Alzheimer%26%23x2019%3Bs%20disease%20%7C%20SpringerLink.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Flink.springer.com%5C%2Farticle%5C%2F10.1186%5C%2F1471-2202-9-S2-S16%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Flink.springer.com%5C%2Farticle%5C%2F10.1186%5C%2F1471-2202-9-S2-S16%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Hypometabolism%20as%20a%20therapeutic%20target%20in%20Alzheimer%27s%20disease%20%7C%20SpringerLink%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flink.springer.com%5C%2Farticle%5C%2F10.1186%5C%2F1471-2202-9-S2-S16%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T11%3A48%3A44Z%22%7D%7D%2C%7B%22key%22%3A%22VCPKRBSX%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDietary%20ketosis%20enhances%20memory%20in%20mild%20cognitive%20impairment%20-%20ScienceDirect.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fabs%5C%2Fpii%5C%2FS0197458010004392%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fabs%5C%2Fpii%5C%2FS0197458010004392%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Dietary%20ketosis%20enhances%20memory%20in%20mild%20cognitive%20impairment%20-%20ScienceDirect%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fabs%5C%2Fpii%5C%2FS0197458010004392%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T11%3A46%3A44Z%22%7D%7D%2C%7B%22key%22%3A%22BDH7M7EZ%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAlzheimer%26%23x2019%3Bs%20Disease%20is%20Type%203%20Diabetes%26%23x2014%3BEvidence%20Reviewed%20-%20Suzanne%20M.%20de%20la%20Monte%2C%20Jack%20R.%20Wands%2C%202008.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fjournals.sagepub.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1177%5C%2F193229680800200619%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fjournals.sagepub.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1177%5C%2F193229680800200619%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Alzheimer%27s%20Disease%20is%20Type%203%20Diabetes%5Cu2014Evidence%20Reviewed%20-%20Suzanne%20M.%20de%20la%20Monte%2C%20Jack%20R.%20Wands%2C%202008%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fjournals.sagepub.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1177%5C%2F193229680800200619%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T11%3A42%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22RWXZB9WD%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFeasibility%20and%20efficacy%20data%20from%20a%20ketogenic%20diet%20intervention%20in%20Alzheimer%26%23x2019%3Bs%20disease%20-%20ScienceDirect.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS2352873717300707%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS2352873717300707%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Feasibility%20and%20efficacy%20data%20from%20a%20ketogenic%20diet%20intervention%20in%20Alzheimer%27s%20disease%20-%20ScienceDirect%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS2352873717300707%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T11%3A27%3A13Z%22%7D%7D%2C%7B%22key%22%3A%22E7CGIUQT%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Pawlosky%20et%20al.%22%2C%22parsedDate%22%3A%222020-02-04%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPawlosky%20RJ%2C%20Kashiwaya%20Y%2C%20King%20MT%2C%20Veech%20RL%20%282020%29%20A%20Dietary%20Ketone%20Ester%20Normalizes%20Abnormal%20Behavior%20in%20a%20Mouse%20Model%20of%20Alzheimer%26%23x2019%3Bs%20Disease.%20IJMS%2021%3A1044.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijms21031044%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijms21031044%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20Dietary%20Ketone%20Ester%20Normalizes%20Abnormal%20Behavior%20in%20a%20Mouse%20Model%20of%20Alzheimer%5Cu2019s%20Disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%20J.%22%2C%22lastName%22%3A%22Pawlosky%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoshihero%22%2C%22lastName%22%3A%22Kashiwaya%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20Todd%22%2C%22lastName%22%3A%22King%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20L.%22%2C%22lastName%22%3A%22Veech%22%7D%5D%2C%22abstractNote%22%3A%22Because%20of%20a%20decreased%20sensitivity%20toward%20insulin%2C%20a%20key%20regulator%20of%20pyruvate%20dehydrogenase%20%28PDH%29%2C%20Alzheimer%5Cu2019s%20patients%20have%20lower%20brain%20glucose%20utilization%20with%20reductions%20in%20Tricarboxylic%20Acid%20%28TCA%29%20cycle%20metabolites%20such%20as%20citrate%2C%20a%20precursor%20to%20n-acetyl-aspartate.%20In%20the%203xTgAd%20mouse%20model%20of%20Alzheimer%5Cu2019s%20disease%20%28AD%29%2C%20aging%20mice%20also%20demonstrate%20low%20brain%20glucose%20metabolism.%20Ketone%20metabolism%20can%20overcome%20PDH%20inhibition%20and%20restore%20TCA%20cycle%20metabolites%2C%20thereby%20enhancing%20amino%20acid%20biosynthesis.%20A%20ketone%20ester%20of%20d-%5Cu03b2-hydroxybutyrate%20was%20incorporated%20into%20a%20diet%20%28Ket%29%20and%20fed%20to%203xTgAd%20mice.%20A%20control%20group%20was%20fed%20a%20calorically%20matched%20diet%20%28Cho%29.%20At%2015%20months%20of%20age%2C%20the%20exploratory%20and%20avoidance-related%20behavior%20patterns%20of%20the%20mice%20were%20evaluated.%20At%2016.5%20months%20of%20age%2C%20the%20animals%20were%20euthanized%2C%20and%20their%20hippocampi%20were%20analyzed%20for%20citrate%2C%20%5Cu03b1-ketoglutarate%2C%20and%20amino%20acids.%20In%20the%20hippocampi%20of%20the%20Ket-fed%20mice%2C%20there%20were%20higher%20concentrations%20of%20citrate%20and%20%5Cu03b1-ketoglutarate%20as%20well%20as%20higher%20concentrations%20of%20glutamate%2C%20aspartate%20and%20n-acetyl-aspartate%20compared%20with%20controls.%20There%20were%20positive%20associations%20between%20%281%29%20concentrations%20of%20aspartate%20and%20n-acetyl-aspartate%20%28n%20%3D%2014%2C%20R%20%3D%200.9327%29%2C%20and%20%282%29%20%5Cu03b1-ketoglutarate%20and%20glutamate%20%28n%20%3D%2014%2C%20R%20%3D%200.8521%29%20in%20animals%20maintained%20on%20either%20diet.%20Hippocampal%20n-acetyl-aspartate%20predicted%20the%20outcome%20of%20several%20exploratory%20and%20avoidance-related%20behaviors.%20Ketosis%20restored%20citrate%20and%20%5Cu03b1-ketoglutarate%20in%20the%20hippocampi%20of%20aging%20mice.%20Higher%20concentrations%20of%20n-acetyl-aspartate%20corresponded%20with%20greater%20exploratory%20activity%20and%20reduced%20avoidance-related%20behavior.%22%2C%22date%22%3A%222020-02-04%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fijms21031044%22%2C%22ISSN%22%3A%221422-0067%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F1422-0067%5C%2F21%5C%2F3%5C%2F1044%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T11%3A22%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22N7L4Y9YZ%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rafi%20and%20Alavi%22%2C%22parsedDate%22%3A%222017-08-30%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRafi%20MA%2C%20Alavi%20A%20%282017%29%20Debate%20on%20human%20aging%20and%20lifespan.%20Bioimpacts%207%3A135%26%23x2013%3B137.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.15171%5C%2Fbi.2017.16%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.15171%5C%2Fbi.2017.16%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Debate%20on%20human%20aging%20and%20lifespan%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mohammad%20A.%22%2C%22lastName%22%3A%22Rafi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Abass%22%2C%22lastName%22%3A%22Alavi%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222017-08-30%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.15171%5C%2Fbi.2017.16%22%2C%22ISSN%22%3A%222228-5660%2C%202228-5652%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fbi.tbzmed.ac.ir%5C%2FAbstract%5C%2Fbi-17493%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A48%3A50Z%22%7D%7D%2C%7B%22key%22%3A%22EX3J7PVP%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Crimmins%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCrimmins%20EM%20%282015%29%20Lifespan%20and%20Healthspan%3A%20Past%2C%20Present%2C%20and%20Promise.%20GERONT%2055%3A901%26%23x2013%3B911.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Fgeront%5C%2Fgnv130%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Fgeront%5C%2Fgnv130%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Lifespan%20and%20Healthspan%3A%20Past%2C%20Present%2C%20and%20Promise%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eileen%20M.%22%2C%22lastName%22%3A%22Crimmins%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2212%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1093%5C%2Fgeront%5C%2Fgnv130%22%2C%22ISSN%22%3A%220016-9013%2C%201758-5341%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Facademic.oup.com%5C%2Fgerontologist%5C%2Farticle-lookup%5C%2Fdoi%5C%2F10.1093%5C%2Fgeront%5C%2Fgnv130%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A48%3A09Z%22%7D%7D%2C%7B%22key%22%3A%223JWL79XX%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Huang%20and%20Mark%20Jacquez%22%2C%22parsedDate%22%3A%222017-05-28%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHuang%20Y%2C%20Mark%20Jacquez%20G%20%282017%29%20Identification%20of%20a%20Blue%20Zone%20in%20a%20Typical%20Chinese%20Longevity%20Region.%20IJERPH%2014%3A571.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijerph14060571%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijerph14060571%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Identification%20of%20a%20Blue%20Zone%20in%20a%20Typical%20Chinese%20Longevity%20Region%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yi%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Geoffrey%22%2C%22lastName%22%3A%22Mark%20Jacquez%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222017-05-28%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fijerph14060571%22%2C%22ISSN%22%3A%221660-4601%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F1660-4601%5C%2F14%5C%2F6%5C%2F571%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A44%3A11Z%22%7D%7D%2C%7B%22key%22%3A%22BBWNJ6WM%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Poulain%20et%20al.%22%2C%22parsedDate%22%3A%222004%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPoulain%20M%2C%20Pes%20GM%2C%20Grasland%20C%2C%20et%20al%20%282004%29%20Identification%20of%20a%20geographic%20area%20characterized%20by%20extreme%20longevity%20in%20the%20Sardinia%20island%3A%20the%20AKEA%20study.%20Experimental%20Gerontology%2039%3A1423%26%23x2013%3B1429.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.exger.2004.06.016%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.exger.2004.06.016%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Identification%20of%20a%20geographic%20area%20characterized%20by%20extreme%20longevity%20in%20the%20Sardinia%20island%3A%20the%20AKEA%20study%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michel%22%2C%22lastName%22%3A%22Poulain%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Giovanni%20Mario%22%2C%22lastName%22%3A%22Pes%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Claude%22%2C%22lastName%22%3A%22Grasland%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ciriaco%22%2C%22lastName%22%3A%22Carru%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Luigi%22%2C%22lastName%22%3A%22Ferrucci%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Giovannella%22%2C%22lastName%22%3A%22Baggio%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Claudio%22%2C%22lastName%22%3A%22Franceschi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Luca%22%2C%22lastName%22%3A%22Deiana%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%229%5C%2F2004%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.exger.2004.06.016%22%2C%22ISSN%22%3A%2205315565%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0531556504002141%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A42%3A41Z%22%7D%7D%2C%7B%22key%22%3A%22BWIHNYER%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BMetabolic%20Syndrome%20and%20Risk%20of%20Cancer%20%7C%20Diabetes%20Care.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fcare.diabetesjournals.org%5C%2Fcontent%5C%2F35%5C%2F11%5C%2F2402.abstract%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fcare.diabetesjournals.org%5C%2Fcontent%5C%2F35%5C%2F11%5C%2F2402.abstract%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Metabolic%20Syndrome%20and%20Risk%20of%20Cancer%20%7C%20Diabetes%20Care%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fcare.diabetesjournals.org%5C%2Fcontent%5C%2F35%5C%2F11%5C%2F2402.abstract%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A26%3A51Z%22%7D%7D%2C%7B%22key%22%3A%22HIHTSGMM%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Esposito%20et%20al.%22%2C%22parsedDate%22%3A%222012-11-01%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BEsposito%20K%2C%20Chiodini%20P%2C%20Colao%20A%2C%20et%20al%20%282012%29%20Metabolic%20Syndrome%20and%20Risk%20of%20Cancer%3A%20A%20systematic%20review%20and%20meta-analysis.%20Diabetes%20Care%2035%3A2402%26%23x2013%3B2411.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.2337%5C%2Fdc12-0336%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.2337%5C%2Fdc12-0336%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Metabolic%20Syndrome%20and%20Risk%20of%20Cancer%3A%20A%20systematic%20review%20and%20meta-analysis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%22%2C%22lastName%22%3A%22Esposito%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Chiodini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Colao%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Lenzi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Giugliano%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVEdAvailable%20evidence%20supports%20the%20emerging%20hypothesis%20that%20metabolic%20syndrome%20may%20be%20associated%20with%20the%20risk%20of%20some%20common%20cancers.%20We%20did%20a%20systematic%20review%20and%20metaanalysis%20to%20assess%20the%20association%20between%20metabolic%20syndrome%20and%20risk%20of%20cancer%20at%20different%20sites.%20RESEARCH%20DESIGN%20AND%20METHODSdWe%20conducted%20an%20electronic%20search%20for%20articles%20published%20through%20October%202011%20without%20restrictions%20and%20by%20reviewing%20reference%20lists%20from%20retrieved%20articles.%20Every%20included%20study%20was%20to%20report%20risk%20estimates%20with%2095%25%20CIs%20for%20the%20association%20between%20metabolic%20syndrome%20and%20cancer.%5CnRESULTSdWe%20analyzed%20116%20datasets%20from%2043%20articles%2C%20including%2038%2C940%20cases%20of%20cancer.%20In%20cohort%20studies%20in%20men%2C%20the%20presence%20of%20metabolic%20syndrome%20was%20associated%20with%20liver%20%28relative%20risk%201.43%2C%20P%20%2C%200.0001%29%2C%20colorectal%20%281.25%2C%20P%20%2C%200.001%29%2C%20and%20bladder%20cancer%20%281.10%2C%20P%20%3D%200.013%29.%20In%20cohort%20studies%20in%20women%2C%20the%20presence%20of%20metabolic%20syndrome%20was%20associated%20with%20endometrial%20%281.61%2C%20P%20%3D%200.001%29%2C%20pancreatic%20%281.58%2C%20P%20%2C%200.0001%29%2C%20breast%20postmenopausal%20%281.56%2C%20P%20%3D%200.017%29%2C%20rectal%20%281.52%2C%20P%20%3D%200.005%29%2C%20and%20colorectal%20%281.34%2C%20P%20%3D%200.006%29%20cancers.%20Associations%20with%20metabolic%20syndrome%20were%20stronger%20in%20women%20than%20in%20men%20for%20pancreatic%20%28P%20%3D%200.01%29%20and%20rectal%20%28P%20%3D%200.01%29%20cancers.%20Associations%20were%20different%20between%20ethnic%20groups%3A%20we%20recorded%20stronger%20associations%20in%20Asia%20populations%20for%20liver%20cancer%20%28P%20%3D%200.002%29%2C%20in%20European%20populations%20for%20colorectal%20cancer%20in%20women%20%28P%20%3D%200.004%29%2C%20and%20in%20U.S.%20populations%20%28whites%29%20for%20prostate%20cancer%20%28P%20%3D%200.001%29.%5CnCONCLUSIONSdMetabolic%20syndrome%20is%20associated%20with%20increased%20risk%20of%20common%20cancers%3B%20for%20some%20cancers%2C%20the%20risk%20differs%20betweens%20sexes%2C%20populations%2C%20and%20de%5Cufb01nitions%20of%20metabolic%20syndrome.%22%2C%22date%22%3A%222012-11-01%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.2337%5C%2Fdc12-0336%22%2C%22ISSN%22%3A%220149-5992%2C%201935-5548%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fcare.diabetesjournals.org%5C%2Fcgi%5C%2Fdoi%5C%2F10.2337%5C%2Fdc12-0336%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A26%3A40Z%22%7D%7D%2C%7B%22key%22%3A%22NJAIXK92%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BObesity%20and%20Risk%20of%20Cancer%3A%20An%20Introductory%20Overview%20%7C%20SpringerLink.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Flink.springer.com%5C%2Fchapter%5C%2F10.1007%5C%2F978-3-319-42542-9_1%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Flink.springer.com%5C%2Fchapter%5C%2F10.1007%5C%2F978-3-319-42542-9_1%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2030%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Obesity%20and%20Risk%20of%20Cancer%3A%20An%20Introductory%20Overview%20%7C%20SpringerLink%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flink.springer.com%5C%2Fchapter%5C%2F10.1007%5C%2F978-3-319-42542-9_1%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A20%3A58Z%22%7D%7D%2C%7B%22key%22%3A%22V5LNMCKW%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Seeman%20et%20al.%22%2C%22parsedDate%22%3A%222004%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSeeman%20TE%2C%20Crimmins%20E%2C%20Huang%20M-H%2C%20et%20al%20%282004%29%20Cumulative%20biological%20risk%20and%20socio-economic%20differences%20in%20mortality%3A%20MacArthur%20Studies%20of%20Successful%20Aging.%20Social%20Science%20%26amp%3B%20Medicine%2058%3A1985%26%23x2013%3B1997.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2FS0277-9536%2803%2900402-7%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2FS0277-9536%2803%2900402-7%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Cumulative%20biological%20risk%20and%20socio-economic%20differences%20in%20mortality%3A%20MacArthur%20Studies%20of%20Successful%20Aging%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Teresa%20E%22%2C%22lastName%22%3A%22Seeman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eileen%22%2C%22lastName%22%3A%22Crimmins%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mei-Hua%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Burton%22%2C%22lastName%22%3A%22Singer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alexander%22%2C%22lastName%22%3A%22Bucur%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tara%22%2C%22lastName%22%3A%22Gruenewald%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lisa%20F%22%2C%22lastName%22%3A%22Berkman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%20B%22%2C%22lastName%22%3A%22Reuben%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%225%5C%2F2004%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2FS0277-9536%2803%2900402-7%22%2C%22ISSN%22%3A%2202779536%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0277953603004027%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A18%3A50Z%22%7D%7D%2C%7B%22key%22%3A%22HCF2WDQ2%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Pinquart%20and%20S%5Cu00f6rensen%22%2C%22parsedDate%22%3A%222000%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPinquart%20M%2C%20S%26%23xF6%3Brensen%20S%20%282000%29%20Influences%20of%20socioeconomic%20status%2C%20social%20network%2C%20and%20competence%20on%20subjective%20well-being%20in%20later%20life%3A%20A%20meta-analysis.%20Psychology%20and%20Aging%2015%3A187%26%23x2013%3B224.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1037%5C%2F0882-7974.15.2.187%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1037%5C%2F0882-7974.15.2.187%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Influences%20of%20socioeconomic%20status%2C%20social%20network%2C%20and%20competence%20on%20subjective%20well-being%20in%20later%20life%3A%20A%20meta-analysis.%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Martin%22%2C%22lastName%22%3A%22Pinquart%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Silvia%22%2C%22lastName%22%3A%22S%5Cu00f6rensen%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222000%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1037%5C%2F0882-7974.15.2.187%22%2C%22ISSN%22%3A%221939-1498%2C%200882-7974%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdoi.apa.org%5C%2Fgetdoi.cfm%3Fdoi%3D10.1037%5C%2F0882-7974.15.2.187%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A18%3A43Z%22%7D%7D%2C%7B%22key%22%3A%22JT22QG53%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Orzack%20et%20al.%22%2C%22parsedDate%22%3A%222015-04-21%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BOrzack%20SH%2C%20Stubblefield%20JW%2C%20Akmaev%20VR%2C%20et%20al%20%282015%29%20The%20human%20sex%20ratio%20from%20conception%20to%20birth.%20Proc%20Natl%20Acad%20Sci%20USA%20112%3AE2102%26%23x2013%3BE2111.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1416546112%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1416546112%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20human%20sex%20ratio%20from%20conception%20to%20birth%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%20Hecht%22%2C%22lastName%22%3A%22Orzack%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20William%22%2C%22lastName%22%3A%22Stubblefield%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Viatcheslav%20R.%22%2C%22lastName%22%3A%22Akmaev%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Pere%22%2C%22lastName%22%3A%22Colls%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Santiago%22%2C%22lastName%22%3A%22Munn%5Cu00e9%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thomas%22%2C%22lastName%22%3A%22Scholl%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%22%2C%22lastName%22%3A%22Steinsaltz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20E.%22%2C%22lastName%22%3A%22Zuckerman%22%7D%5D%2C%22abstractNote%22%3A%22We%20describe%20the%20trajectory%20of%20the%20human%20sex%20ratio%20from%20conception%20to%20birth%20by%20analyzing%20data%20from%20%28%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20i%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20%29%203-%20to%206-d-old%20embryos%2C%20%28%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20ii%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20%29%20induced%20abortions%2C%20%28%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20iii%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20%29%20chorionic%20villus%20sampling%2C%20%28%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20iv%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20%29%20amniocentesis%2C%20and%20%28%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20v%5Cn%20%20%20%20%20%20%20%20%20%20%20%20%20%20%29%20fetal%20deaths%20and%20live%20births.%20Our%20dataset%20is%20the%20most%20comprehensive%20and%20largest%20ever%20assembled%20to%20estimate%20the%20sex%20ratio%20at%20conception%20and%20the%20sex%20ratio%20trajectory%20and%20is%20the%20first%2C%20to%20our%20knowledge%2C%20to%20include%20all%20of%20these%20types%20of%20data.%20Our%20estimate%20of%20the%20sex%20ratio%20at%20conception%20is%200.5%20%28proportion%20male%29%2C%20which%20contradicts%20the%20common%20claim%20that%20the%20sex%20ratio%20at%20conception%20is%20male-biased.%20The%20sex%20ratio%20among%20abnormal%20embryos%20is%20male-biased%2C%20and%20the%20sex%20ratio%20among%20normal%20embryos%20is%20female-biased.%20These%20biases%20are%20associated%20with%20the%20abnormal%5C%2Fnormal%20state%20of%20the%20sex%20chromosomes%20and%20of%20chromosomes%2015%20and%2017.%20The%20sex%20ratio%20may%20decrease%20in%20the%20first%20week%20or%20so%20after%20conception%20%28due%20to%20excess%20male%20mortality%29%3B%20it%20then%20increases%20for%20at%20least%2010%5Cu201315%20wk%20%28due%20to%20excess%20female%20mortality%29%2C%20levels%20off%20after%20%5Cu223c20%20wk%2C%20and%20declines%20slowly%20from%2028%20to%2035%20wk%20%28due%20to%20excess%20male%20mortality%29.%20Total%20female%20mortality%20during%20pregnancy%20exceeds%20total%20male%20mortality.%20The%20unbiased%20sex%20ratio%20at%20conception%2C%20the%20increase%20in%20the%20sex%20ratio%20during%20the%20first%20trimester%2C%20and%20total%20mortality%20during%20pregnancy%20being%20greater%20for%20females%20are%20fundamental%20insights%20into%20early%20human%20development.%22%2C%22date%22%3A%222015-04-21%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1073%5C%2Fpnas.1416546112%22%2C%22ISSN%22%3A%220027-8424%2C%201091-6490%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.pnas.org%5C%2Flookup%5C%2Fdoi%5C%2F10.1073%5C%2Fpnas.1416546112%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A06%3A36Z%22%7D%7D%2C%7B%22key%22%3A%22EG2K9KAT%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Austad%22%2C%22parsedDate%22%3A%222015-04-21%22%2C%22numChildren%22%3A3%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAustad%20SN%20%282015%29%20The%20human%20prenatal%20sex%20ratio%3A%20A%20major%20surprise.%20PNAS%20112%3A4839%26%23x2013%3B4840.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1505165112%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1505165112%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20human%20prenatal%20sex%20ratio%3A%20A%20major%20surprise%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%20N.%22%2C%22lastName%22%3A%22Austad%22%7D%5D%2C%22abstractNote%22%3A%22Two%20remarkably%20consistent%20and%20poorly%20understood%20features%20of%20human%20biology%20are%20the%20slightly%20male-biased%20sex%20ratio%20at%20birth%20and%20the%20female%20survival%20advantage%20throughout%20life.%20These%20patterns%20appear%20across%20geography%20and%20time%20wherever%20reliable%20birth%20and%20death%20records%20are%20available%20%281%2C%202%29.%20The%20slight%20male%20bias%2C%20typically%20%5Cu223c51.3%25%20of%20live%20births%2C%20is%20so%20consistent%20%28Fig.%201%20A%20%29%20that%20when%20birth%20sex%20ratios%20deviate%20much%20from%20it%2C%20suspicions%20are%20aroused%20of%20sex-specific%20abortion%20or%20infanticide%20%283%2C%204%29.%20Putting%20together%20the%20birth%20sex%20ratio%20bias%20and%20the%20female%20survival%20advantage%20%285%29%2C%20we%20expect%20a%20monotonically%20declining%20sex%20ratio%20from%20birth%20to%20death%2C%20which%20is%20exactly%20what%20we%20find%20across%20cultures%20and%20across%20historical%20epochs%20%28Fig.%201%20B%20%29.%20By%20age%20100%20y%2C%20there%20are%20three%20to%20four%20women%20for%20every%20surviving%20man%2C%20and%20by%20the%20extraordinary%20age%20of%20110%20y%2C%2095%25%20of%20the%20survivors%20are%20women.%20Note%2C%20however%2C%20that%20until%20later%20life%20the%20sex%20ratio%20does%20not%20stray%20far%20from%2050%3A50%2C%20an%20observation%20that%20would%20gladden%20the%20heart%20of%20evolutionary%20biologist%2C%20Sir%20Ronald%20Fisher%2C%20who%20argued%20that%20natural%20selection%20should%20favor%20equal%20parental%20expenditure%5Cu2014a%20delightfully%20vague%20phrase%5Cu2014in%20males%20and%20females%20%286%29.%20Fisher%20assumed%2C%20as%20have%20many%20since%20then%2C%20that%20the%20human%20sex%20ratio%20at%20conception%20is%20even%20more%20male-biased%20than%20the%20sex%20ratio%20at%20birth%2C%20and%20there%20were%20some%20good%20reasons%20to%20assume%20this.%20First%2C%20males%20are%20less%20likely%20%5Cu2026%20%5Cn%5Cn%5B%5Cu21b5%5D%5B1%5D1Email%3A%20austad%7Bat%7Duab.edu.%5Cn%5Cn%20%5B1%5D%3A%20%23xref-corresp-1-1%22%2C%22date%22%3A%222015%5C%2F04%5C%2F21%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1073%5C%2Fpnas.1505165112%22%2C%22ISSN%22%3A%220027-8424%2C%201091-6490%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.pnas.org%5C%2Fcontent%5C%2F112%5C%2F16%5C%2F4839%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A05%3A43Z%22%7D%7D%2C%7B%22key%22%3A%2298E6DTMD%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Austad%20and%20Fischer%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAustad%20SN%2C%20Fischer%20KE%20%282016%29%20Sex%20Differences%20in%20Lifespan.%20Cell%20Metabolism%2023%3A1022%26%23x2013%3B1033.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cmet.2016.05.019%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cmet.2016.05.019%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Sex%20Differences%20in%20Lifespan%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%20N.%22%2C%22lastName%22%3A%22Austad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kathleen%20E.%22%2C%22lastName%22%3A%22Fischer%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2206%5C%2F2016%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.cmet.2016.05.019%22%2C%22ISSN%22%3A%2215504131%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS1550413116302376%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T10%3A00%3A37Z%22%7D%7D%2C%7B%22key%22%3A%224S3DHHQN%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lema%5Cu00eetre%20et%20al.%22%2C%22parsedDate%22%3A%222020-03-23%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLema%26%23xEE%3Btre%20J-F%2C%20Ronget%20V%2C%20Tidi%26%23xE8%3Bre%20M%2C%20et%20al%20%282020%29%20Sex%20differences%20in%20adult%20lifespan%20and%20aging%20rates%20of%20mortality%20across%20wild%20mammals.%20Proc%20Natl%20Acad%20Sci%20USA.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1911999117%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1073%5C%2Fpnas.1911999117%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Sex%20differences%20in%20adult%20lifespan%20and%20aging%20rates%20of%20mortality%20across%20wild%20mammals%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jean-Fran%5Cu00e7ois%22%2C%22lastName%22%3A%22Lema%5Cu00eetre%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Victor%22%2C%22lastName%22%3A%22Ronget%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Morgane%22%2C%22lastName%22%3A%22Tidi%5Cu00e8re%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dominique%22%2C%22lastName%22%3A%22Allain%5Cu00e9%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22V%5Cu00e9rane%22%2C%22lastName%22%3A%22Berger%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aur%5Cu00e9lie%22%2C%22lastName%22%3A%22Cohas%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fernando%22%2C%22lastName%22%3A%22Colchero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dalia%20A.%22%2C%22lastName%22%3A%22Conde%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%22%2C%22lastName%22%3A%22Garratt%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andr%5Cu00e1s%22%2C%22lastName%22%3A%22Liker%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gabriel%20A.%20B.%22%2C%22lastName%22%3A%22Marais%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alexander%22%2C%22lastName%22%3A%22Scheuerlein%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tam%5Cu00e1s%22%2C%22lastName%22%3A%22Sz%5Cu00e9kely%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jean-Michel%22%2C%22lastName%22%3A%22Gaillard%22%7D%5D%2C%22abstractNote%22%3A%22In%20human%20populations%2C%20women%20consistently%20outlive%20men%2C%20which%20suggests%20profound%20biological%20foundations%20for%20sex%20differences%20in%20survival.%20Quantifying%20whether%20such%20sex%20differences%20are%20also%20pervasive%20in%20wild%20mammals%20is%20a%20crucial%20challenge%20in%20both%20evolutionary%20biology%20and%20biogerontology.%20Here%2C%20we%20compile%20demographic%20data%20from%20134%20mammal%20populations%2C%20encompassing%20101%20species%2C%20to%20show%20that%20the%20female%26%23039%3Bs%20median%20lifespan%20is%20on%20average%2018.6%25%20longer%20than%20that%20of%20conspecific%20males%2C%20whereas%20in%20humans%20the%20female%20advantage%20is%20on%20average%207.8%25.%20On%20the%20contrary%2C%20we%20do%20not%20find%20any%20consistent%20sex%20differences%20in%20aging%20rates.%20In%20addition%2C%20sex%20differences%20in%20median%20adult%20lifespan%20and%20aging%20rates%20are%20both%20highly%20variable%20across%20species.%20Our%20analyses%20suggest%20that%20the%20magnitude%20of%20sex%20differences%20in%20mammalian%20mortality%20patterns%20is%20likely%20shaped%20by%20local%20environmental%20conditions%20in%20interaction%20with%20the%20sex-specific%20costs%20of%20sexual%20selection.%22%2C%22date%22%3A%22Mar%2023%2C%202020%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1073%5C%2Fpnas.1911999117%22%2C%22ISSN%22%3A%221091-6490%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-30T09%3A47%3A09Z%22%7D%7D%2C%7B%22key%22%3A%22B6QAFUMT%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zanoboni%20et%20al.%22%2C%22parsedDate%22%3A%221976-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BZanoboni%20A%2C%20Schwarz%20D%2C%20Zanoboni-Muciaccia%20W%20%281976%29%20Stimulation%20of%20insulin%20secretion%20in%20man%20by%20oral%20glycerol%20administration.%20Metab%20Clin%20Exp%2025%3A41%26%23x2013%3B45.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2F0026-0495%2876%2990158-x%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2F0026-0495%2876%2990158-x%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Stimulation%20of%20insulin%20secretion%20in%20man%20by%20oral%20glycerol%20administration%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Zanoboni%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Schwarz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W.%22%2C%22lastName%22%3A%22Zanoboni-Muciaccia%22%7D%5D%2C%22abstractNote%22%3A%22The%20effects%20of%20an%20orally%20administered%20glycerol%20load%20%281%20g%5C%2FKg%20body%20weight%29%20on%20blood%20glucose%2C%20plasma%20FFA%2C%20and%20plasma%20insulin%20levels%20have%20been%20determined%20in%20eight%20normal%20fasting%20or%20glucose%20loaded%20%281%20g%5C%2FKg%20body%20weight%29%20volunteers.%20Blood%20glucose%20levels%20were%20not%20affected%20by%20glycerol%20loading%20while%20glicemia%20followed%20the%20same%20pattern%20of%20a%20glucose%20tolerance%20test%20in%20the%20group%20treated%20with%20glucose%20plus%20glycerol.%20Plasma%20FFA%20were%20significantly%20lowered%20only%2090%20min%20after%20glycerol%20loading%20while%20they%20had%20markedly%20and%20persistently%20decreased%20by%20glycerol%20plus%20glucose%20per%20os.%20Finally%2C%20though%20glicemia%20did%20not%20change%2C%20insulinemia%20was%20markedly%20increased%20by%20glycereol%2C%2090%20min%20after%20loading%3B%20moreover%2C%20plasma%20IRI%20was%20significantly%20higher%20in%20the%20group%20treated%20with%20glycerol%20plus%20glucose%20than%20in%20the%20group%20treated%20with%20glucose%20alone.%20These%20data%20suggest%20that%20the%20release%20of%20insulin%20may%20be%20stimulated%20by%20a%20very%20small%20increment%20of%20blood%20glucose%2C%20which%20derives%20from%20glycerol.%22%2C%22date%22%3A%22Jan%201976%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1016%5C%2F0026-0495%2876%2990158-x%22%2C%22ISSN%22%3A%220026-0495%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%226ZD5MYAL%22%5D%2C%22dateModified%22%3A%222020-03-29T14%3A53%3A22Z%22%7D%7D%2C%7B%22key%22%3A%22KC29XC9H%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAssociation%20of%20Triglyceride-Lowering%20LPL%20Variants%20and%20LDL-C%26%23x2013%3BLowering%20LDLR%20Variants%20With%20Risk%20of%20Coronary%20Heart%20Disease%20%7C%20Cardiology%20%7C%20JAMA%20%7C%20JAMA%20Network.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fjamanetwork.com%5C%2Fjournals%5C%2Fjama%5C%2Farticle-abstract%5C%2F2722770%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fjamanetwork.com%5C%2Fjournals%5C%2Fjama%5C%2Farticle-abstract%5C%2F2722770%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2029%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Association%20of%20Triglyceride-Lowering%20LPL%20Variants%20and%20LDL-C%5Cu2013Lowering%20LDLR%20Variants%20With%20Risk%20of%20Coronary%20Heart%20Disease%20%7C%20Cardiology%20%7C%20JAMA%20%7C%20JAMA%20Network%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fjamanetwork.com%5C%2Fjournals%5C%2Fjama%5C%2Farticle-abstract%5C%2F2722770%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-29T10%3A39%3A29Z%22%7D%7D%2C%7B%22key%22%3A%22N98JYWCU%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Madsen%20et%20al.%22%2C%22parsedDate%22%3A%222008%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BMadsen%20EL%2C%20Rissanen%20A%2C%20Bruun%20JM%2C%20et%20al%20%282008%29%20Weight%20loss%20larger%20than%2010%25%20is%20needed%20for%20general%20improvement%20of%20levels%20of%20circulating%20adiponectin%20and%20markers%20of%20inflammation%20in%20obese%20subjects%3A%20a%203-year%20weight%20loss%20study.%20European%20Journal%20of%20Endocrinology%20158%3A179%26%23x2013%3B187.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1530%5C%2FEJE-07-0721%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1530%5C%2FEJE-07-0721%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Weight%20loss%20larger%20than%2010%25%20is%20needed%20for%20general%20improvement%20of%20levels%20of%20circulating%20adiponectin%20and%20markers%20of%20inflammation%20in%20obese%20subjects%3A%20a%203-year%20weight%20loss%20study%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erik%20L%22%2C%22lastName%22%3A%22Madsen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aila%22%2C%22lastName%22%3A%22Rissanen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jens%20M%22%2C%22lastName%22%3A%22Bruun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kristin%22%2C%22lastName%22%3A%22Skogstrand%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Serena%22%2C%22lastName%22%3A%22Tonstad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%20M%22%2C%22lastName%22%3A%22Hougaard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bj%5Cu00f8rn%22%2C%22lastName%22%3A%22Richelsen%22%7D%5D%2C%22abstractNote%22%3A%22Objective%3A%20To%20investigate%20the%20effects%20of%3A%20I%29%20short-%20%288%20weeks%29%2C%20II%29%20long-term%20%283%20years%29%20weight%20loss%2C%20and%20III%29%20the%20degree%20of%20weight%20loss%20on%20circulating%20levels%20of%20adiponectin%2C%20high%20sensitive-C%20reactive%20protein%20%28hs-CRP%29%2C%20and%20%5Cufb01brinogen%20in%20obese%20subjects.%20Moreover%2C%20to%20evaluate%20the%20effect%20of%20the%20lipase%20inhibitor%2C%20orlistat%2C%20on%20these%20parameters.%20Design%3A%20Weight%20loss%20induced%20in%2093%20obese%20subjects%20%28mean%20weight%3A%20108.9G15.8%20kg%29%20through%208-week%20very-low-energy%20diet%20%28VLED%2C%20800%20kcal%5C%2Fday%29%20followed%20by%20randomization%20to%20orlistat%20or%20placebo%20together%20with%20lifestyle%20intervention%20for%20further%203%20years.%20Adiponectin%20and%20hs-CRP%20were%20measured%20at%20baseline%2C%20after%208%20weeks%20of%20VLED%20and%206%2C%2012%2C%20and%2036%20months%20after%20the%20VLED%20by%20%5Cufb02owmetric%20xMAP%20technology%20%28Luminex%20Multi-Analyte%20Pro%5Cufb01ling%20System%2C%20Luminex%20Corp.%2C%20Austin%2C%20TX%2C%20USA%29.%20Fibrinogen%20was%20measured%20in%20a%20coagulation%20assay.%5CnResults%3A%20Weight%20loss%20after%20VLED%20treatment%20was%2014.3G4.5%20kg%20and%20after%203%20years%207.7G8.7%20kg.%20Orlistattreated%20subjects%20regained%203.9%20kg%20less%20than%20placebo-treated%20from%20the%20end%20of%20the%20VLED%20to%203%20years%20%28PZ0.01%29.%20No%20differences%20were%20detected%20between%20the%20two%20groups%20regarding%20changes%20in%20adiponectin%2C%20hs-CRP%2C%20or%20%5Cufb01brinogen.%20Accordingly%2C%20the%20groups%20were%20combined%20for%20further%20analyses.%20Serum%20adiponectin%20increased%20by%2022%25%20%28P%210.05%29%20after%20the%20VLED%20but%20returned%20to%20baseline%20after%203%20years.%20Both%20short-%20and%20long-term%20weight%20losses%20needed%20to%20be%20in%20excess%20of%2010%25%20%28w12%20kg%29%20in%20order%20to%20increase%20adiponectin%20levels%20signi%5Cufb01cantly.%20Weight%20loss%20was%20associated%20with%20a%20signi%5Cufb01cant%20decrease%20in%20hs-CRP.%20Fibrinogen%20decreased%20by%2012%25%20%28P%210.05%29%20after%203%20years.%5CnConclusions%3A%20In%20obese%20subjects%2C%20weight%20loss%20was%20associated%20with%20an%20increase%20in%20serum%20adiponectin%20and%20a%20decrease%20in%20hs-CRP%20and%20plasma%20%5Cufb01brinogen.%20Long-term%20weight%20loss%20%283%20years%29%20must%20exceed%2010%25%20to%20induce%20a%20combined%20signi%5Cufb01cant%20improvement%20in%20these%20in%5Cufb02ammatory%20markers.%22%2C%22date%22%3A%2202%5C%2F2008%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1530%5C%2FEJE-07-0721%22%2C%22ISSN%22%3A%220804-4643%2C%201479-683X%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Feje.bioscientifica.com%5C%2Fview%5C%2Fjournals%5C%2Feje%5C%2F158%5C%2F2%5C%2F179.xml%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-26T18%3A25%3A24Z%22%7D%7D%2C%7B%22key%22%3A%22ZAHCKML2%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Danesh%20et%20al.%22%2C%22parsedDate%22%3A%222000-07-22%22%2C%22numChildren%22%3A3%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDanesh%20J%2C%20Whincup%20P%2C%20Walker%20M%2C%20et%20al%20%282000%29%20Low%20grade%20inflammation%20and%20coronary%20heart%20disease%3A%20prospective%20study%20and%20updated%20meta-analyses.%20BMJ%20321%3A199%26%23x2013%3B204.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1136%5C%2Fbmj.321.7255.199%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1136%5C%2Fbmj.321.7255.199%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Low%20grade%20inflammation%20and%20coronary%20heart%20disease%3A%20prospective%20study%20and%20updated%20meta-analyses%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%22%2C%22lastName%22%3A%22Danesh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Peter%22%2C%22lastName%22%3A%22Whincup%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mary%22%2C%22lastName%22%3A%22Walker%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lucy%22%2C%22lastName%22%3A%22Lennon%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrew%22%2C%22lastName%22%3A%22Thomson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Paul%22%2C%22lastName%22%3A%22Appleby%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20Ruth%22%2C%22lastName%22%3A%22Gallimore%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mark%20B.%22%2C%22lastName%22%3A%22Pepys%22%7D%5D%2C%22abstractNote%22%3A%22Objective%3A%20To%20assess%20associations%20between%20baseline%20values%20of%20four%20different%20circulating%20markers%20of%20inflammation%20and%20future%20risk%20of%20coronary%20heart%20disease%2C%20potential%20triggers%20of%20systemic%20inflammation%20%28such%20as%20persistent%20infection%29%2C%20and%20other%20markers%20of%20inflammation.%5CnDesign%3A%20Nested%20case-control%20comparisons%20in%20a%20prospective%2C%20population%20based%20cohort.%5CnSetting%3A%20General%20practices%20in%2018%20towns%20in%20Britain.%5CnParticipants%3A%20506%20men%20who%20died%20from%20coronary%20heart%20disease%20or%20had%20a%20non-fatal%20myocardial%20infarction%20and%201025%20men%20who%20remained%20free%20of%20such%20disease%20until%201996%20selected%20from%205661%20men%20aged%2040%5Cu201359%20years%20who%20provided%20blood%20samples%20in%201978-1980.%5CnMain%20outcome%20measures%3A%20Plasma%20concentrations%20of%20C%20reactive%20protein%2C%20serum%20amyloid%20A%20protein%2C%20and%20serum%20albumin%20and%20leucocyte%20count.%20Information%20on%20fatal%20and%20non-fatal%20coronary%20heart%20disease%20was%20obtained%20from%20medical%20records%20and%20death%20certificates.%5CnResults%3A%20Compared%20with%20men%20in%20the%20bottom%20third%20of%20baseline%20measurements%20of%20C%20reactive%20protein%2C%20men%20in%20the%20top%20third%20had%20an%20odds%20ratio%20for%20coronary%20heart%20disease%20of%202.13%20%2895%25%20confidence%20interval%201.38%20to%203.28%29%20after%20age%2C%20town%2C%20smoking%2C%20vascular%20risk%20factors%2C%20and%20indicators%20of%20socioeconomic%20status%20were%20adjusted%20for.%20Similar%20adjusted%20odds%20ratios%20were%201.65%20%281.07%20to%202.55%29%20for%20serum%20amyloid%20A%20protein%3B%201.12%20%280.71%20to%201.77%29%20for%20leucocyte%20count%3B%20and%200.67%20%280.43%20to%201.04%29%20for%20albumin.%20No%20strong%20associations%20were%20observed%20of%20these%20factors%20with%20Helicobacter%20pylori%20seropositivity%2C%20Chlamydia%20pneumoniae%20IgG%20titres%2C%20or%20plasma%20total%20homocysteine%20concentrations.%20Baseline%20values%20of%20the%20acute%20phase%20reactants%20were%20significantly%20associated%20with%20one%20another%20%28P%26lt%3B0.0001%29%2C%20although%20the%20association%20between%20low%20serum%20albumin%20concentration%20and%20leucocyte%20count%20was%20weaker%20%28P%3D0.08%29.%5CnConclusion%3A%20In%20the%20context%20of%20results%20from%20other%20relevant%20studies%20these%20findings%20suggest%20that%20some%20inflammatory%20processes%2C%20unrelated%20to%20the%20chronic%20infections%20studied%20here%2C%20are%20likely%20to%20be%20involved%20in%20coronary%20heart%20disease.%22%2C%22date%22%3A%222000%5C%2F07%5C%2F22%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1136%5C%2Fbmj.321.7255.199%22%2C%22ISSN%22%3A%220959-8138%2C%201468-5833%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.bmj.com%5C%2Fcontent%5C%2F321%5C%2F7255%5C%2F199%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-26T18%3A13%3A11Z%22%7D%7D%2C%7B%22key%22%3A%22BZZFC7M4%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Nguyen%20et%20al.%22%2C%22parsedDate%22%3A%222010-09-01%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNguyen%20NT%2C%20Nguyen%20X-MT%2C%20Wooldridge%20JB%2C%20et%20al%20%282010%29%20Association%20of%20obesity%20with%20risk%20of%20coronary%20heart%20disease%3A%20findings%20from%20the%20National%20Health%20and%20Nutrition%20Examination%20Survey%2C%201999%26%23x2013%3B2006.%20Surgery%20for%20Obesity%20and%20Related%20Diseases%206%3A465%26%23x2013%3B469.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.soard.2010.02.038%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.soard.2010.02.038%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Association%20of%20obesity%20with%20risk%20of%20coronary%20heart%20disease%3A%20findings%20from%20the%20National%20Health%20and%20Nutrition%20Examination%20Survey%2C%201999%5Cu20132006%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ninh%20T.%22%2C%22lastName%22%3A%22Nguyen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xuan-Mai%20T.%22%2C%22lastName%22%3A%22Nguyen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20B.%22%2C%22lastName%22%3A%22Wooldridge%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Johnathan%20A.%22%2C%22lastName%22%3A%22Slone%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%20S.%22%2C%22lastName%22%3A%22Lane%22%7D%5D%2C%22abstractNote%22%3A%22Background%5CnObesity%20is%20a%20well-known%20risk%20factor%20for%20the%20development%20of%20coronary%20heart%20disease%20%28CHD%29.%20The%20aim%20of%20the%20present%20study%20was%20to%20examine%20the%20differences%20in%20the%2010-year%20CHD%20risk%20with%20increasing%20severity%20of%20obesity%20in%20men%20and%20women%20participating%20in%20the%20latest%20National%20Health%20and%20Nutrition%20Examination%20Survey.%5CnMethods%5CnData%20from%20a%20representative%20sample%20of%2012%2C500%20U.S.%20participants%20in%20the%20National%20Health%20and%20Nutrition%20Examination%20Survey%20from%201999%20to%202006%20were%20reviewed.%20The%20Framingham%20risk%20score%20was%20calculated%20for%20men%20and%20women%20according%20to%20a%20body%20mass%20index%20%28BMI%29%20of%20%26lt%3B25.0%2C%2025.0%5Cu201329.9%2C%2030.0%5Cu201334.9%2C%20and%20%5Cu226535.0%20kg%5C%2Fm2.%5CnResults%5CnThe%20prevalence%20of%20those%20with%20hypertension%20increased%20with%20an%20increasing%20BMI%2C%20from%2024%25%20for%20a%20BMI%20%26lt%3B25.0%20kg%5C%2Fm2%20to%2054%25%20for%20a%20BMI%20of%20%5Cu226535.0%20kg%5C%2Fm2.%20The%20prevalence%20of%20an%20abnormal%20total%20cholesterol%20level%20%28%26gt%3B200%20mg%5C%2FdL%29%20increased%20from%2040%25%20for%20a%20BMI%20%26lt%3B25.0%20kg%5C%2Fm2%20to%2048%25%20for%20a%20BMI%20of%20%5Cu226535.0%20kg%5C%2Fm2.%20The%2010-year%20CHD%20risk%20for%20men%20increased%20from%203.1%25%20for%20a%20BMI%20%26lt%3B25.0%20kg%5C%2Fm2%20to%20a%20peak%20of%205.6%25%20for%20a%20BMI%20of%2030.0%5Cu201334.9%20kg%5C%2Fm2.%20The%2010-year%20CHD%20risk%20for%20women%20increased%20from%20.8%25%20for%20a%20BMI%20%26lt%3B25.0%20kg%5C%2Fm2%20to%20a%20peak%20of%201.5%25%20for%20a%20BMI%20of%20%5Cu226535.0%20kg%5C%2Fm2.%20Both%20diabetes%20and%20hypertension%20were%20independent%20risk%20factors%20for%20an%20increasing%20CHD%20risk.%5CnConclusions%5CnThe%2010-year%20CHD%20risk%2C%20calculated%20using%20the%20Framingham%20risk%20score%2C%20substantially%20increased%20with%20an%20increasing%20BMI.%20An%20important%20implication%20from%20our%20findings%20is%20the%20need%20to%20implement%20surgical%20and%20medical%20approaches%20to%20weight%20reduction%20to%20reduce%20the%20effect%20of%20morbidity%20and%20mortality%20from%20CHD%20on%20the%20U.S.%20healthcare%20system.%22%2C%22date%22%3A%22September%201%2C%202010%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.soard.2010.02.038%22%2C%22ISSN%22%3A%221550-7289%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS155072891000078X%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-26T18%3A06%3A04Z%22%7D%7D%2C%7B%22key%22%3A%226QAPJYLP%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Partsalaki%20et%20al.%22%2C%22parsedDate%22%3A%222012%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPartsalaki%20I%2C%20Karvela%20A%2C%20Spiliotis%20BE%20%282012%29%20Metabolic%20impact%20of%20a%20ketogenic%20diet%20compared%20to%20a%20hypocaloric%20diet%20in%20obese%20children%20and%20adolescents.%20J%20Pediatr%20Endocrinol%20Metab%2025%3A697%26%23x2013%3B704.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1515%5C%2Fjpem-2012-0131%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1515%5C%2Fjpem-2012-0131%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Metabolic%20impact%20of%20a%20ketogenic%20diet%20compared%20to%20a%20hypocaloric%20diet%20in%20obese%20children%20and%20adolescents%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ioanna%22%2C%22lastName%22%3A%22Partsalaki%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alexia%22%2C%22lastName%22%3A%22Karvela%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bessie%20E.%22%2C%22lastName%22%3A%22Spiliotis%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20The%20effects%20of%20carbohydrate-restricted%20%28ketogenic%29%20diets%20on%20metabolic%20parameters%20in%20children%20have%20been%20incompletely%20assessed.%5CnOBJECTIVE%3A%20To%20compare%20the%20efficacy%20and%20metabolic%20impact%20of%20ketogenic%20and%20hypocaloric%20diets%20in%20obese%20children%20and%20adolescents.%5CnSUBJECTS%3A%20Fifty-eight%20obese%20subjects%20were%20placed%20on%20one%20of%20the%20two%20diets%20for%206%20months.%5CnMETHODS%3A%20Anthropometric%20measurements%2C%20body%20composition%2C%20oral%20glucose%5C%2Finsulin%20tolerance%20test%2C%20lipidemic%20profile%2C%20high%20molecular%20weight%20%28HMW%29%20adiponectin%2C%20whole-body%20insulin%20sensitivity%20index%20%28WBISI%29%2C%20and%20homeostatic%20model%20assessment-insulin%20resistance%20%28HOMA-IR%29%20were%20determined%20before%20and%20after%20each%20diet.%5CnRESULTS%3A%20Both%20groups%20significantly%20reduced%20their%20weight%2C%20fat%20mass%2C%20waist%20circumference%2C%20fasting%20insulin%2C%20and%20HOMA-IR%20%28p%20%3D%200.009%20for%20ketogenic%20and%20p%20%3D%200.014%20for%20hypocaloric%29%2C%20but%20the%20differences%20were%20greater%20in%20the%20ketogenic%20group.%20Both%20groups%20increased%20WBISI%20significantly%2C%20but%20only%20the%20ketogenic%20group%20increased%20HMW%20adiponectin%20significantly%20%28p%20%3D%200.025%29.%5CnCONCLUSIONS%3A%20The%20ketogenic%20diet%20revealed%20more%20pronounced%20improvements%20in%20weight%20loss%20and%20metabolic%20parameters%20than%20the%20hypocaloric%20diet%20and%20may%20be%20a%20feasible%20and%20safe%20alternative%20for%20children%26%23039%3Bs%20weight%20loss.%22%2C%22date%22%3A%222012%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1515%5C%2Fjpem-2012-0131%22%2C%22ISSN%22%3A%220334-018X%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%5D%2C%22dateModified%22%3A%222020-03-26T18%3A01%3A30Z%22%7D%7D%2C%7B%22key%22%3A%2269H39AXY%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Volek%20et%20al.%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BVolek%20J%2C%20Phinney%20S%2C%20Forsythe%20C%2C%20et%20al%20%283%29%20%28PDF%29%20Carbohydrate%20Restriction%20has%20a%20More%20Favorable%20Impact%20on%20the%20Metabolic%20Syndrome%20than%20a%20Low%20Fat%20Diet.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.researchgate.net%5C%2Fpublication%5C%2F23663658_Carbohydrate_Restriction_has_a_More_Favorable_Impact_on_the_Metabolic_Syndrome_than_a_Low_Fat_Diet%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.researchgate.net%5C%2Fpublication%5C%2F23663658_Carbohydrate_Restriction_has_a_More_Favorable_Impact_on_the_Metabolic_Syndrome_than_a_Low_Fat_Diet%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2026%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22%283%29%20%28PDF%29%20Carbohydrate%20Restriction%20has%20a%20More%20Favorable%20Impact%20on%20the%20Metabolic%20Syndrome%20than%20a%20Low%20Fat%20Diet%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J%22%2C%22lastName%22%3A%22Volek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stephen%22%2C%22lastName%22%3A%22Phinney%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cassandra%22%2C%22lastName%22%3A%22Forsythe%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erin%22%2C%22lastName%22%3A%22Quinn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%22%2C%22lastName%22%3A%22Wood%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%22%2C%22lastName%22%3A%22Puglisi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22William%20J%22%2C%22lastName%22%3A%22Kraemer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Doug%22%2C%22lastName%22%3A%22Bibus%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20Luz%22%2C%22lastName%22%3A%22Fernandez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20D%22%2C%22lastName%22%3A%22Feinman%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.researchgate.net%5C%2Fpublication%5C%2F23663658_Carbohydrate_Restriction_has_a_More_Favorable_Impact_on_the_Metabolic_Syndrome_than_a_Low_Fat_Diet%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22TX7VNSFI%22%5D%2C%22dateModified%22%3A%222020-03-26T17%3A58%3A42Z%22%7D%7D%2C%7B%22key%22%3A%22S7I9MHTC%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKeto%20Longevity%20Webinar.%20In%3A%20Google%20Docs.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdocs.google.com%5C%2Fdocument%5C%2Fu%5C%2F1%5C%2Fd%5C%2F1uD7YzT94lPqTYB00DGyKEDuQNjp0TOKKGv5d1s6dbdI%5C%2Fedit%3Fusp%3Dsharing%26amp%3Busp%3Dembed_facebook%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdocs.google.com%5C%2Fdocument%5C%2Fu%5C%2F1%5C%2Fd%5C%2F1uD7YzT94lPqTYB00DGyKEDuQNjp0TOKKGv5d1s6dbdI%5C%2Fedit%3Fusp%3Dsharing%26amp%3Busp%3Dembed_facebook%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2026%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Keto%20Longevity%20Webinar%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22Title%3A%20Can%20You%20Extend%20Your%20Lifespan%20With%20a%20Ketogenic%20Diet%3F%20%20Intro%3A%20The%20Guaranteed%20Ketogenic%20Diet%20%20Part%201%3A%20How%20Long%20Can%20You%20Expect%20to%20Live%3F%20How%20long%20does%20the%20average%20person%20live%3F%20-%20Erin%20Gender%20differences%20Location%20How%20much%20influenced%20by%20diet%20itself%3F%20Socioeconomic%3F%20How%20much%20can%20we%20impact%3F%20Genetics%3F...%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fdocs.google.com%5C%2Fdocument%5C%2Fu%5C%2F1%5C%2Fd%5C%2F1uD7YzT94lPqTYB00DGyKEDuQNjp0TOKKGv5d1s6dbdI%5C%2Fedit%3Fusp%3Dsharing%26usp%3Dembed_facebook%22%2C%22language%22%3A%22en-GB%22%2C%22collections%22%3A%5B%5D%2C%22dateModified%22%3A%222020-03-26T17%3A28%3A14Z%22%7D%7D%2C%7B%22key%22%3A%22W7HE8HHJ%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wilson%20et%20al.%22%2C%22parsedDate%22%3A%222005-11-15%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWilson%20PWF%2C%20D%26%23x2019%3BAgostino%20RB%2C%20Parise%20H%2C%20et%20al%20%282005%29%20Metabolic%20Syndrome%20as%20a%20Precursor%20of%20Cardiovascular%20Disease%20and%20Type%202%20Diabetes%20Mellitus.%20Circulation%20112%3A3066%26%23x2013%3B3072.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1161%5C%2FCIRCULATIONAHA.105.539528%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1161%5C%2FCIRCULATIONAHA.105.539528%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Metabolic%20Syndrome%20as%20a%20Precursor%20of%20Cardiovascular%20Disease%20and%20Type%202%20Diabetes%20Mellitus%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Peter%20W.F.%22%2C%22lastName%22%3A%22Wilson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ralph%20B.%22%2C%22lastName%22%3A%22D%5Cu2019Agostino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helen%22%2C%22lastName%22%3A%22Parise%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lisa%22%2C%22lastName%22%3A%22Sullivan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20B.%22%2C%22lastName%22%3A%22Meigs%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222005-11-15%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1161%5C%2FCIRCULATIONAHA.105.539528%22%2C%22ISSN%22%3A%220009-7322%2C%201524-4539%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ahajournals.org%5C%2Fdoi%5C%2F10.1161%5C%2FCIRCULATIONAHA.105.539528%22%2C%22collections%22%3A%5B%5D%2C%22dateModified%22%3A%222020-03-26T17%3A09%3A36Z%22%7D%7D%2C%7B%22key%22%3A%22T65RIIYX%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gershuni%20et%20al.%22%2C%22parsedDate%22%3A%222018-09-01%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BGershuni%20VM%2C%20Yan%20SL%2C%20Medici%20V%20%282018%29%20Nutritional%20Ketosis%20for%20Weight%20Management%20and%20Reversal%20of%20Metabolic%20Syndrome.%20Curr%20Nutr%20Rep%207%3A97%26%23x2013%3B106.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs13668-018-0235-0%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs13668-018-0235-0%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Nutritional%20Ketosis%20for%20Weight%20Management%20and%20Reversal%20of%20Metabolic%20Syndrome%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Victoria%20M.%22%2C%22lastName%22%3A%22Gershuni%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stephanie%20L.%22%2C%22lastName%22%3A%22Yan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Valentina%22%2C%22lastName%22%3A%22Medici%22%7D%5D%2C%22abstractNote%22%3A%22The%20goal%20of%20this%20paper%20is%20to%20review%20current%20literature%20on%20nutritional%20ketosis%20within%20the%20context%20of%20weight%20management%20and%20metabolic%20syndrome%2C%20namely%2C%20insulin%20resistance%2C%20lipid%20profile%2C%20cardiovascular%20disease%20risk%2C%20and%20development%20of%20non-alcoholic%20fatty%20liver%20disease.%20We%20provide%20background%20on%20the%20mechanism%20of%20ketogenesis%20and%20describe%20nutritional%20ketosis.%22%2C%22date%22%3A%222018-09-01%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1007%5C%2Fs13668-018-0235-0%22%2C%22ISSN%22%3A%222161-3311%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs13668-018-0235-0%22%2C%22collections%22%3A%5B%226GWVSRHP%22%5D%2C%22dateModified%22%3A%222020-03-26T16%3A54%3A11Z%22%7D%7D%2C%7B%22key%22%3A%226NT2M8NW%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Volek%20and%20Sharman%22%2C%22parsedDate%22%3A%222004%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BVolek%20JS%2C%20Sharman%20MJ%20%282004%29%20Cardiovascular%20and%20Hormonal%20Aspects%20of%20Very-Low-Carbohydrate%20Ketogenic%20Diets.%20Obesity%20Research%2012%3A115S-123S.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Foby.2004.276%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Foby.2004.276%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Cardiovascular%20and%20Hormonal%20Aspects%20of%20Very-Low-Carbohydrate%20Ketogenic%20Diets%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeff%20S.%22%2C%22lastName%22%3A%22Volek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Matthew%20J.%22%2C%22lastName%22%3A%22Sharman%22%7D%5D%2C%22abstractNote%22%3A%22VOLEK%2C%20JEFF%20S.%20AND%20MATTHEW%20J.%20SHARMAN.%20Cardiovascular%20and%20hormonal%20aspects%20of%20very-lowcarbohydrate%20ketogenic%20diets.%20Obes%20Res.%202004%3B12%3A%20115S%5Cu2013123S.%22%2C%22date%22%3A%2211%5C%2F2004%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1038%5C%2Foby.2004.276%22%2C%22ISSN%22%3A%2210717323%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdoi.wiley.com%5C%2F10.1038%5C%2Foby.2004.276%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-19T17%3A34%3A29Z%22%7D%7D%2C%7B%22key%22%3A%223BUZRYYF%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kosinski%20and%20Jornayvaz%22%2C%22parsedDate%22%3A%222017-05-19%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKosinski%20C%2C%20Jornayvaz%20F%20%282017%29%20Effects%20of%20Ketogenic%20Diets%20on%20Cardiovascular%20Risk%20Factors%3A%20Evidence%20from%20Animal%20and%20Human%20Studies.%20Nutrients%209%3A517.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu9050517%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu9050517%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Effects%20of%20Ketogenic%20Diets%20on%20Cardiovascular%20Risk%20Factors%3A%20Evidence%20from%20Animal%20and%20Human%20Studies%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christophe%22%2C%22lastName%22%3A%22Kosinski%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fran%5Cu00e7ois%22%2C%22lastName%22%3A%22Jornayvaz%22%7D%5D%2C%22abstractNote%22%3A%22The%20treatment%20of%20obesity%20and%20cardiovascular%20diseases%20is%20one%20of%20the%20most%20dif%5Cufb01cult%20and%20important%20challenges%20nowadays.%20Weight%20loss%20is%20frequently%20offered%20as%20a%20therapy%20and%20is%20aimed%20at%20improving%20some%20of%20the%20components%20of%20the%20metabolic%20syndrome.%20Among%20various%20diets%2C%20ketogenic%20diets%2C%20which%20are%20very%20low%20in%20carbohydrates%20and%20usually%20high%20in%20fats%20and%5C%2For%20proteins%2C%20have%20gained%20in%20popularity.%20Results%20regarding%20the%20impact%20of%20such%20diets%20on%20cardiovascular%20risk%20factors%20are%20controversial%2C%20both%20in%20animals%20and%20humans%2C%20but%20some%20improvements%20notably%20in%20obesity%20and%20type%202%20diabetes%20have%20been%20described.%20Unfortunately%2C%20these%20effects%20seem%20to%20be%20limited%20in%20time.%20Moreover%2C%20these%20diets%20are%20not%20totally%20safe%20and%20can%20be%20associated%20with%20some%20adverse%20events.%20Notably%2C%20in%20rodents%2C%20development%20of%20nonalcoholic%20fatty%20liver%20disease%20%28NAFLD%29%20and%20insulin%20resistance%20have%20been%20described.%20The%20aim%20of%20this%20review%20is%20to%20discuss%20the%20role%20of%20ketogenic%20diets%20on%20different%20cardiovascular%20risk%20factors%20in%20both%20animals%20and%20humans%20based%20on%20available%20evidence.%22%2C%22date%22%3A%222017-05-19%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fnu9050517%22%2C%22ISSN%22%3A%222072-6643%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F2072-6643%5C%2F9%5C%2F5%5C%2F517%22%2C%22collections%22%3A%5B%229P7SYM5Z%22%5D%2C%22dateModified%22%3A%222020-03-19T17%3A25%3A20Z%22%7D%7D%2C%7B%22key%22%3A%22QYCRY2WY%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rusek%20et%20al.%22%2C%22parsedDate%22%3A%222019-08-09%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRusek%20M%2C%20Pluta%20R%2C%20U%26%23x142%3Bamek-Kozio%26%23x142%3B%20M%2C%20Czuczwar%20SJ%20%282019%29%20Ketogenic%20Diet%20in%20Alzheimer%26%23x2019%3Bs%20Disease.%20IJMS%2020%3A3892.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijms20163892%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fijms20163892%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Ketogenic%20Diet%20in%20Alzheimer%5Cu2019s%20Disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marta%22%2C%22lastName%22%3A%22Rusek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ryszard%22%2C%22lastName%22%3A%22Pluta%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marzena%22%2C%22lastName%22%3A%22U%5Cu0142amek-Kozio%5Cu0142%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stanis%5Cu0142aw%20J.%22%2C%22lastName%22%3A%22Czuczwar%22%7D%5D%2C%22abstractNote%22%3A%22At%20present%2C%20the%20prevalence%20of%20Alzheimer%5Cu2019s%20disease%2C%20a%20devastating%20neurodegenerative%20disorder%2C%20is%20increasing.%20Although%20the%20mechanism%20of%20the%20underlying%20pathology%20is%20not%20fully%20uncovered%2C%20in%20the%20last%20years%2C%20there%20has%20been%20signi%5Cufb01cant%20progress%20in%20its%20understanding.%20This%20includes%3A%20Progressive%20deposition%20of%20amyloid%20%5Cu03b2-peptides%20in%20amyloid%20plaques%20and%20hyperphosphorylated%20tau%20protein%20in%20intracellular%20as%20neuro%5Cufb01brillary%20tangles%3B%20neuronal%20loss%3B%20and%20impaired%20glucose%20metabolism.%20Due%20to%20a%20lack%20of%20e%5Cufb00ective%20prevention%20and%20treatment%20strategy%2C%20emerging%20evidence%20suggests%20that%20dietary%20and%20metabolic%20interventions%20could%20potentially%20target%20these%20issues.%20The%20ketogenic%20diet%20is%20a%20very%20high-fat%2C%20low-carbohydrate%20diet%2C%20which%20has%20a%20fasting-like%20e%5Cufb00ect%20bringing%20the%20body%20into%20a%20state%20of%20ketosis.%20The%20presence%20of%20ketone%20bodies%20has%20a%20neuroprotective%20impact%20on%20aging%20brain%20cells.%20Moreover%2C%20their%20production%20may%20enhance%20mitochondrial%20function%2C%20reduce%20the%20expression%20of%20in%5Cufb02ammatory%20and%20apoptotic%20mediators.%20Thus%2C%20it%20has%20gained%20interest%20as%20a%20potential%20therapy%20for%20neurodegenerative%20disorders%20like%20Alzheimer%5Cu2019s%20disease.%20This%20review%20aims%20to%20examine%20the%20role%20of%20the%20ketogenic%20diet%20in%20Alzheimer%5Cu2019s%20disease%20progression%20and%20to%20outline%20speci%5Cufb01c%20aspects%20of%20the%20nutritional%20pro%5Cufb01le%20providing%20a%20rationale%20for%20the%20implementation%20of%20dietary%20interventions%20as%20a%20therapeutic%20strategy%20for%20Alzheimer%5Cu2019s%20disease.%22%2C%22date%22%3A%222019-08-09%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fijms20163892%22%2C%22ISSN%22%3A%221422-0067%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F1422-0067%5C%2F20%5C%2F16%5C%2F3892%22%2C%22collections%22%3A%5B%22SPT2NJ53%22%5D%2C%22dateModified%22%3A%222020-03-19T17%3A15%3A25Z%22%7D%7D%2C%7B%22key%22%3A%22BNDJSCA5%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22W%5Cu0142odarek%22%2C%22parsedDate%22%3A%222019-01-15%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BW%26%23x142%3Bodarek%20D%20%282019%29%20Role%20of%20Ketogenic%20Diets%20in%20Neurodegenerative%20Diseases%20%28Alzheimer%26%23x2019%3Bs%20Disease%20and%20Parkinson%26%23x2019%3Bs%20Disease%29.%20Nutrients%2011%3A169.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu11010169%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu11010169%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Role%20of%20Ketogenic%20Diets%20in%20Neurodegenerative%20Diseases%20%28Alzheimer%5Cu2019s%20Disease%20and%20Parkinson%5Cu2019s%20Disease%29%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dariusz%22%2C%22lastName%22%3A%22W%5Cu0142odarek%22%7D%5D%2C%22abstractNote%22%3A%22The%20goal%20of%20this%20review%20was%20to%20assess%20the%20effectiveness%20of%20ketogenic%20diets%20on%20the%20therapy%20of%20neurodegenerative%20diseases.%20The%20ketogenic%20diet%20is%20a%20low-carbohydrate%20and%20fat-rich%20diet.%20Its%20implementation%20has%20a%20fasting-like%20effect%2C%20which%20brings%20the%20body%20into%20a%20state%20of%20ketosis.%20The%20ketogenic%20diet%20has%2C%20for%20almost%20100%20years%2C%20been%20used%20in%20the%20therapy%20of%20drug-resistant%20epilepsy%2C%20but%20current%20studies%20indicate%20possible%20neuroprotective%20effects.%20Thus%20far%2C%20only%20a%20few%20studies%20have%20evaluated%20the%20role%20of%20the%20ketogenic%20diet%20in%20the%20prevention%20of%20Parkinson%5Cu2019s%20disease%20%28PD%29%20and%20Alzheimer%5Cu2019s%20disease%20%28AD%29.%20Single%20studies%20with%20human%20participants%20have%20demonstrated%20a%20reduction%20of%20disease%20symptoms%20after%20application.%20The%20application%20of%20the%20ketogenic%20diet%20to%20elderly%20people%2C%20however%2C%20raises%20certain%20concerns.%20Persons%20with%20neurodegenerative%20diseases%20are%20at%20risk%20of%20malnutrition%2C%20while%20food%20intake%20reduction%20is%20associated%20with%20disease%20symptoms.%20In%20turn%2C%20the%20ketogenic%20diet%20leads%20to%20a%20reduced%20appetite%3B%20it%20is%20not%20attractive%20from%20an%20organoleptic%20point%20of%20view%2C%20and%20may%20be%20accompanied%20by%20side%20effects%20of%20the%20gastrointestinal%20system.%20All%20this%20may%20lead%20to%20further%20lowering%20of%20consumed%20food%20portions%20by%20elderly%20persons%20with%20neurodegenerative%20diseases%20and%2C%20in%20consequence%2C%20to%20further%20reduction%20in%20the%20supply%20of%20nutrients%20provided%20by%20the%20diet.%20Neither%20data%20on%20the%20long-term%20application%20of%20the%20ketogenic%20diet%20in%20patients%20with%20neurodegenerative%20disease%20or%20data%20on%20its%20effects%20on%20disease%20symptoms%20are%20available.%20Further%20research%20is%20needed%20to%20evaluate%20the%20suitability%20of%20the%20ketogenic%20diet%20in%20the%20therapy%20of%20AD-%20or%20PD-affected%20persons.%22%2C%22date%22%3A%222019-01-15%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fnu11010169%22%2C%22ISSN%22%3A%222072-6643%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F2072-6643%5C%2F11%5C%2F1%5C%2F169%22%2C%22collections%22%3A%5B%22SPT2NJ53%22%5D%2C%22dateModified%22%3A%222020-03-19T17%3A07%3A06Z%22%7D%7D%2C%7B%22key%22%3A%22Q6VKADKU%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRole%20of%20Ketogenic%20Diets%20in%20Neurodegenerative%20Diseases%20%28Alzheimer%26%23x2019%3Bs%20Disease%20and%20Parkinson%26%23x2019%3Bs%20Disease%29.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC6356942%5C%2F%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC6356942%5C%2F%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Role%20of%20Ketogenic%20Diets%20in%20Neurodegenerative%20Diseases%20%28Alzheimer%5Cu2019s%20Disease%20and%20Parkinson%5Cu2019s%20Disease%29%22%2C%22creators%22%3A%5B%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC6356942%5C%2F%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%5D%2C%22dateModified%22%3A%222020-03-19T17%3A01%3A10Z%22%7D%7D%2C%7B%22key%22%3A%228YKAEID7%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Fine%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFine%20E%20Targeting%20insulin%20inhibition%20as%20a%20metabolic%20therapy%20in%20advanced%20cancer%3A%20a%20pilot%20safety%20and%20feasibility%20dietary%20trial%20in%2010%20patients.%20-%20PubMed%20-%20NCBI.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F22840388%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F22840388%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Targeting%20insulin%20inhibition%20as%20a%20metabolic%20therapy%20in%20advanced%20cancer%3A%20a%20pilot%20safety%20and%20feasibility%20dietary%20trial%20in%2010%20patients.%20-%20PubMed%20-%20NCBI%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E%22%2C%22lastName%22%3A%22Fine%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F22840388%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A57%3A25Z%22%7D%7D%2C%7B%22key%22%3A%229EYTNPQ2%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zhou%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BZhou%20W%20The%20calorically%20restricted%20ketogenic%20diet%2C%20an%20effective%20alternative%20therapy%20for%20malignant%20brain%20cancer.%20-%20PubMed%20-%20NCBI.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F17313687%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F17313687%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22The%20calorically%20restricted%20ketogenic%20diet%2C%20an%20effective%20alternative%20therapy%20for%20malignant%20brain%20cancer.%20-%20PubMed%20-%20NCBI%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W%22%2C%22lastName%22%3A%22Zhou%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F17313687%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A51%3A30Z%22%7D%7D%2C%7B%22key%22%3A%22Q7HKJ46T%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Klement%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKlement%20Anti-Tumor%20Effects%20of%20Ketogenic%20Diets%20in%20Mice%3A%20A%20Meta-Analysis.%20-%20PubMed%20-%20NCBI.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F27159218%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F27159218%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Anti-Tumor%20Effects%20of%20Ketogenic%20Diets%20in%20Mice%3A%20A%20Meta-Analysis.%20-%20PubMed%20-%20NCBI%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22%22%2C%22lastName%22%3A%22Klement%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpubmed%5C%2F27159218%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A45%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22LBX53LKX%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kentaro%20Nakamura%20et%20al.%22%2C%22parsedDate%22%3A%222018-02-14%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKentaro%20Nakamura%2C%20Hidekazu%20Tonouchi%2C%20Akina%20Sasayama%2C%20Kinya%20Ashida%20%282018%29%20A%20Ketogenic%20Formula%20Prevents%20Tumor%20Progression%20and%20Cancer%20Cachexia%20by%20Attenuating%20Systemic%20Inflammation%20in%20Colon%2026%20Tumor-Bearing%20Mice.%20Nutrients%2010%3A206.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu10020206%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3390%5C%2Fnu10020206%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20Ketogenic%20Formula%20Prevents%20Tumor%20Progression%20and%20Cancer%20Cachexia%20by%20Attenuating%20Systemic%20Inflammation%20in%20Colon%2026%20Tumor-Bearing%20Mice%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22name%22%3A%22Kentaro%20Nakamura%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22name%22%3A%22Hidekazu%20Tonouchi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22name%22%3A%22Akina%20Sasayama%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22name%22%3A%22Kinya%20Ashida%22%7D%5D%2C%22abstractNote%22%3A%22Low-carbohydrate%2C%20high-fat%20diets%20%28ketogenic%20diets%29%20might%20prevent%20tumor%20progression%20and%20could%20be%20used%20as%20supportive%20therapy%3B%20however%2C%20few%20studies%20have%20addressed%20the%20effect%20of%20such%20diets%20on%20colorectal%20cancer.%20An%20infant%20formula%20with%20a%20ketogenic%20composition%20%28ketogenic%20formula%3B%20KF%29%20is%20used%20to%20treat%20patients%20with%20refractory%20epilepsy.%20We%20investigated%20the%20effect%20of%20KF%20on%20cancer%20and%20cancer%20cachexia%20in%20colon%20tumor-bearing%20mice.%20Mice%20were%20randomized%20into%20normal%20%28NR%29%2C%20tumor-bearing%20%28TB%29%2C%20and%20ketogenic%20formula%20%28KF%29%20groups.%20Colon%2026%20cells%20were%20inoculated%20subcutaneously%20into%20TB%20and%20KF%20mice.%20The%20NR%20and%20TB%20groups%20received%20a%20standard%20diet%2C%20and%20the%20KF%20mice%20received%20KF%20ad%20libitum.%20KF%20mice%20preserved%20their%20body%2C%20muscle%2C%20and%20carcass%20weights.%20Tumor%20weight%20and%20plasma%20IL-6%20levels%20were%20signi%5Cufb01cantly%20lower%20in%20KF%20mice%20than%20in%20TB%20mice.%20In%20the%20KF%20group%2C%20energy%20intake%20was%20signi%5Cufb01cantly%20higher%20than%20that%20in%20the%20other%20two%20groups.%20Blood%20ketone%20body%20concentrations%20in%20KF%20mice%20were%20signi%5Cufb01cantly%20elevated%2C%20and%20there%20was%20a%20signi%5Cufb01cant%20negative%20correlation%20between%20blood%20ketone%20body%20concentration%20and%20tumor%20weight.%20Therefore%2C%20KF%20may%20suppress%20the%20progression%20of%20cancer%20and%20the%20accompanying%20systemic%20in%5Cufb02ammation%20without%20adverse%20effects%20on%20weight%20gain%2C%20or%20muscle%20mass%2C%20which%20might%20help%20to%20prevent%20cancer%20cachexia.%22%2C%22date%22%3A%222018-02-14%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.3390%5C%2Fnu10020206%22%2C%22ISSN%22%3A%222072-6643%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.mdpi.com%5C%2F2072-6643%5C%2F10%5C%2F2%5C%2F206%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A41%3A20Z%22%7D%7D%2C%7B%22key%22%3A%22CQQ6Y2IM%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lv%20et%20al.%22%2C%22parsedDate%22%3A%222014-12-11%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLv%20M%2C%20Zhu%20X%2C%20Wang%20H%2C%20et%20al%20%282014%29%20Roles%20of%20Caloric%20Restriction%2C%20Ketogenic%20Diet%20and%20Intermittent%20Fasting%20during%20Initiation%2C%20Progression%20and%20Metastasis%20of%20Cancer%20in%20Animal%20Models%3A%20A%20Systematic%20Review%20and%20Meta-Analysis.%20PLoS%20ONE%209%3Ae115147.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0115147%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0115147%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Roles%20of%20Caloric%20Restriction%2C%20Ketogenic%20Diet%20and%20Intermittent%20Fasting%20during%20Initiation%2C%20Progression%20and%20Metastasis%20of%20Cancer%20in%20Animal%20Models%3A%20A%20Systematic%20Review%20and%20Meta-Analysis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mengmeng%22%2C%22lastName%22%3A%22Lv%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xingya%22%2C%22lastName%22%3A%22Zhu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hao%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Feng%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wenxian%22%2C%22lastName%22%3A%22Guan%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Guillermo%20L%5Cu00f3pez%22%2C%22lastName%22%3A%22Lluch%22%7D%5D%2C%22abstractNote%22%3A%22Background%3A%20The%20role%20of%20dietary%20restriction%20regimens%20such%20as%20caloric%20restriction%2C%20ketogenic%20diet%20and%20intermittent%20fasting%20in%20development%20of%20cancers%20has%20been%20detected%20via%20abundant%20preclinical%20experiments.%20However%2C%20the%20conclusions%20are%20controversial.%20We%20aim%20to%20review%20the%20relevant%20animal%20studies%20systematically%20and%20provide%20assistance%20for%20further%20clinical%20studies.%22%2C%22date%22%3A%222014-12-11%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0115147%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0115147%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A34%3A06Z%22%7D%7D%2C%7B%22key%22%3A%22GM7HUCJD%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Poff%20et%20al.%22%2C%22parsedDate%22%3A%222013-06-05%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPoff%20AM%2C%20Ari%20C%2C%20Seyfried%20TN%2C%20D%26%23x2019%3BAgostino%20DP%20%282013%29%20The%20Ketogenic%20Diet%20and%20Hyperbaric%20Oxygen%20Therapy%20Prolong%20Survival%20in%20Mice%20with%20Systemic%20Metastatic%20Cancer.%20PLoS%20ONE%208%3Ae65522.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0065522%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0065522%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20Ketogenic%20Diet%20and%20Hyperbaric%20Oxygen%20Therapy%20Prolong%20Survival%20in%20Mice%20with%20Systemic%20Metastatic%20Cancer%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Angela%20M.%22%2C%22lastName%22%3A%22Poff%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Csilla%22%2C%22lastName%22%3A%22Ari%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thomas%20N.%22%2C%22lastName%22%3A%22Seyfried%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dominic%20P.%22%2C%22lastName%22%3A%22D%5Cu2019Agostino%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Chih-Hsin%22%2C%22lastName%22%3A%22Tang%22%7D%5D%2C%22abstractNote%22%3A%22Introduction%3A%20Abnormal%20cancer%20metabolism%20creates%20a%20glycolytic-dependency%20which%20can%20be%20exploited%20by%20lowering%20glucose%20availability%20to%20the%20tumor.%20The%20ketogenic%20diet%20%28KD%29%20is%20a%20low%20carbohydrate%2C%20high%20fat%20diet%20which%20decreases%20blood%20glucose%20and%20elevates%20blood%20ketones%20and%20has%20been%20shown%20to%20slow%20cancer%20progression%20in%20animals%20and%20humans.%20Abnormal%20tumor%20vasculature%20creates%20hypoxic%20pockets%20which%20promote%20cancer%20progression%20and%20further%20increase%20the%20glycolytic-dependency%20of%20cancers.%20Hyperbaric%20oxygen%20therapy%20%28HBO2T%29%20saturates%20tumors%20with%20oxygen%2C%20reversing%20the%20cancer%20promoting%20effects%20of%20tumor%20hypoxia.%20Since%20these%20non-toxic%20therapies%20exploit%20overlapping%20metabolic%20deficiencies%20of%20cancer%2C%20we%20tested%20their%20combined%20effects%20on%20cancer%20progression%20in%20a%20natural%20model%20of%20metastatic%20disease.%5CnMethods%3A%20We%20used%20the%20firefly%20luciferase-tagged%20VM-M3%20mouse%20model%20of%20metastatic%20cancer%20to%20compare%20tumor%20progression%20and%20survival%20in%20mice%20fed%20standard%20or%20KD%20ad%20libitum%20with%20or%20without%20HBO2T%20%282.5%20ATM%20absolute%2C%2090%20min%2C%203x%5C%2Fweek%29.%20Tumor%20growth%20was%20monitored%20by%20in%20vivo%20bioluminescent%20imaging.%5CnResults%3A%20KD%20alone%20significantly%20decreased%20blood%20glucose%2C%20slowed%20tumor%20growth%2C%20and%20increased%20mean%20survival%20time%20by%2056.7%25%20in%20mice%20with%20systemic%20metastatic%20cancer.%20While%20HBO2T%20alone%20did%20not%20influence%20cancer%20progression%2C%20combining%20the%20KD%20with%20HBO2T%20elicited%20a%20significant%20decrease%20in%20blood%20glucose%2C%20tumor%20growth%20rate%2C%20and%2077.9%25%20increase%20in%20mean%20survival%20time%20compared%20to%20controls.%5CnConclusions%3A%20KD%20and%20HBO2T%20produce%20significant%20anti-cancer%20effects%20when%20combined%20in%20a%20natural%20model%20of%20systemic%20metastatic%20cancer.%20Our%20evidence%20suggests%20that%20these%20therapies%20should%20be%20further%20investigated%20as%20potential%20non-toxic%20treatments%20or%20adjuvant%20therapies%20to%20standard%20care%20for%20patients%20with%20systemic%20metastatic%20disease.%22%2C%22date%22%3A%222013-6-5%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0065522%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0065522%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A29%3A05Z%22%7D%7D%2C%7B%22key%22%3A%22SWT7IIDA%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Poff%20et%20al.%22%2C%22parsedDate%22%3A%222019%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPoff%20A%2C%20Koutnik%20AP%2C%20Egan%20KM%2C%20et%20al%20%282019%29%20Targeting%20the%20Warburg%20effect%20for%20cancer%20treatment%3A%20Ketogenic%20diets%20for%20management%20of%20glioma.%20Seminars%20in%20Cancer%20Biology%2056%3A135%26%23x2013%3B148.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.semcancer.2017.12.011%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.semcancer.2017.12.011%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Targeting%20the%20Warburg%20effect%20for%20cancer%20treatment%3A%20Ketogenic%20diets%20for%20management%20of%20glioma%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Angela%22%2C%22lastName%22%3A%22Poff%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrew%20P.%22%2C%22lastName%22%3A%22Koutnik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kathleen%20M.%22%2C%22lastName%22%3A%22Egan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Solmaz%22%2C%22lastName%22%3A%22Sahebjam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dominic%22%2C%22lastName%22%3A%22D%5Cu2019Agostino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nagi%20B.%22%2C%22lastName%22%3A%22Kumar%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2206%5C%2F2019%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.semcancer.2017.12.011%22%2C%22ISSN%22%3A%221044579X%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS1044579X17301244%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A11%3A01Z%22%7D%7D%2C%7B%22key%22%3A%22GWS8CT5H%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Sremanakova%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSremanakova%20A%20systematic%20review%20of%20the%20use%20of%20ketogenic%20diets%20in%20adult%20patients%20with%20cancer%20-%20Sremanakova%20-%202018%20-%20Journal%20of%20Human%20Nutrition%20and%20Dietetics%20-%20Wiley%20Online%20Library.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1111%5C%2Fjhn.12587%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1111%5C%2Fjhn.12587%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22A%20systematic%20review%20of%20the%20use%20of%20ketogenic%20diets%20in%20adult%20patients%20with%20cancer%20-%20Sremanakova%20-%202018%20-%20Journal%20of%20Human%20Nutrition%20and%20Dietetics%20-%20Wiley%20Online%20Library%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22%22%2C%22lastName%22%3A%22Sremanakova%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2Fabs%5C%2F10.1111%5C%2Fjhn.12587%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A03%3A12Z%22%7D%7D%2C%7B%22key%22%3A%224RDMGN6M%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Bettum%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBettum%20IJ%2C%20Gorad%20SS%2C%20Barkovskaya%20A%2C%20et%20al%20%282015%29%20Metabolic%20reprogramming%20supports%20the%20invasive%20phenotype%20in%20malignant%20melanoma.%20Cancer%20Letters%20366%3A71%26%23x2013%3B83.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.canlet.2015.06.006%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.canlet.2015.06.006%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Metabolic%20reprogramming%20supports%20the%20invasive%20phenotype%20in%20malignant%20melanoma%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ingrid%20J.%22%2C%22lastName%22%3A%22Bettum%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Saurabh%20S.%22%2C%22lastName%22%3A%22Gorad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anna%22%2C%22lastName%22%3A%22Barkovskaya%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Solveig%22%2C%22lastName%22%3A%22Pettersen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Siver%20A.%22%2C%22lastName%22%3A%22Moestue%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kotryna%22%2C%22lastName%22%3A%22Vasiliauskaite%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ellen%22%2C%22lastName%22%3A%22Tenstad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tove%22%2C%22lastName%22%3A%22%5Cu00d8yjord%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22%5Cu00d8ystein%22%2C%22lastName%22%3A%22Risa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vigdis%22%2C%22lastName%22%3A%22Nygaard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gunhild%20M.%22%2C%22lastName%22%3A%22M%5Cu00e6landsmo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lina%22%2C%22lastName%22%3A%22Prasmickaite%22%7D%5D%2C%22abstractNote%22%3A%22Invasiveness%20is%20a%20hallmark%20of%20aggressive%20cancer%20like%20malignant%20melanoma%2C%20and%20factors%20involved%20in%20acquisition%20or%20maintenance%20of%20an%20invasive%20phenotype%20are%20attractive%20targets%20for%20therapy.%20We%20investigated%20melanoma%20phenotype%20modulation%20induced%20by%20the%20metastasis-promoting%20microenvironmental%20protein%20S100A4%2C%20focusing%20on%20the%20relationship%20between%20enhanced%20cellular%20motility%2C%20dedifferentiation%20and%20metabolic%20changes.%20In%20poorly%20motile%2C%20well-differentiated%20Melmet%205%20cells%2C%20S100A4%20stimulated%20migration%2C%20invasion%20and%20simultaneously%20down-regulated%20differentiation%20genes%20and%20modulated%20expression%20of%20metabolism%20genes.%20Metabolic%20studies%20con%5Cufb01rmed%20suppressed%20mitochondrial%20respiration%20and%20activated%20glycolytic%20%5Cufb02ux%20in%20the%20S100A4%20stimulated%20cells%2C%20indicating%20a%20metabolic%20switch%20toward%20aerobic%20glycolysis%2C%20known%20as%20the%20Warburg%20effect.%20Reversal%20of%20the%20glycolytic%20switch%20by%20dichloracetate%20induced%20apoptosis%20and%20reduced%20cell%20growth%2C%20particularly%20in%20the%20S100A4%20stimulated%20cells.%20This%20implies%20that%20cells%20with%20stimulated%20invasiveness%20get%20survival%20bene%5Cufb01t%20from%20the%20glycolytic%20switch%20and%2C%20therefore%2C%20become%20more%20vulnerable%20to%20glycolysis%20inhibition.%20In%20conclusion%2C%20our%20data%20indicate%20that%20transition%20to%20the%20invasive%20phenotype%20in%20melanoma%20involves%20dedifferentiation%20and%20metabolic%20reprogramming%20from%20mitochondrial%20oxidation%20to%20glycolysis%2C%20which%20facilitates%20survival%20of%20the%20invasive%20cancer%20cells.%20Therapeutic%20strategies%20targeting%20the%20metabolic%20reprogramming%20may%20therefore%20be%20effective%20against%20the%20invasive%20phenotype.%22%2C%22date%22%3A%2209%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.canlet.2015.06.006%22%2C%22ISSN%22%3A%2203043835%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0304383515003985%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A01%3A54Z%22%7D%7D%2C%7B%22key%22%3A%22D9QF3U55%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hanahan%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHanahan%20Hallmarks%20of%20Cancer%3A%20The%20Next%20Generation%3A%20Cell.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-ItemURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fwww.cell.com%5C%2Fcell%5C%2Ffulltext%5C%2FS0092-8674%2811%2900127-9%3F_returnURL%3Dhttps%253A%252F%252Flinkinghub.elsevier.com%252Fretrieve%252Fpii%252FS0092867411001279%253Fshowall%253Dtrue%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fwww.cell.com%5C%2Fcell%5C%2Ffulltext%5C%2FS0092-8674%2811%2900127-9%3F_returnURL%3Dhttps%253A%252F%252Flinkinghub.elsevier.com%252Fretrieve%252Fpii%252FS0092867411001279%253Fshowall%253Dtrue%26lt%3B%5C%2Fa%26gt%3B.%20Accessed%2019%20Mar%202020%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22webpage%22%2C%22title%22%3A%22Hallmarks%20of%20Cancer%3A%20The%20Next%20Generation%3A%20Cell%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22%22%2C%22lastName%22%3A%22Hanahan%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.cell.com%5C%2Fcell%5C%2Ffulltext%5C%2FS0092-8674%2811%2900127-9%3F_returnURL%3Dhttps%253A%252F%252Flinkinghub.elsevier.com%252Fretrieve%252Fpii%252FS0092867411001279%253Fshowall%253Dtrue%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T16%3A00%3A21Z%22%7D%7D%2C%7B%22key%22%3A%22BT3F4UR4%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Warburg%22%2C%22parsedDate%22%3A%221956-02-24%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWarburg%20O%20%281956%29%20On%20the%20Origin%20of%20Cancer%20Cells.%20Science%20123%3A309%26%23x2013%3B314.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1126%5C%2Fscience.123.3191.309%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1126%5C%2Fscience.123.3191.309%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22On%20the%20Origin%20of%20Cancer%20Cells%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22O.%22%2C%22lastName%22%3A%22Warburg%22%7D%5D%2C%22abstractNote%22%3A%22Cancer%20cells%20originate%20from%20normal%20body%20cells%20in%20two%20phases.%20The%20first%20phase%20is%20the%20irreversible%20injuring%20of%20respiration.%20Just%20as%20there%20are%20many%20remote%20causes%20of%20plague-heat%2C%20insects%2C%20rats-but%20only%20one%20common%20cause%2C%20the%20plague%20bacillus%2C%20there%20are%20a%20great%20many%20remote%20causes%20of%20cancer-tar%2C%20rays%2C%20arsenic%2C%20pressure%2C%20urethane-but%20there%20is%20only%20one%20common%20cause%20into%20which%20all%20other%20causes%20of%20cancer%20merge%2C%20the%20irreversible%20injuring%20of%20respiration.%22%2C%22date%22%3A%221956-02-24%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1126%5C%2Fscience.123.3191.309%22%2C%22ISSN%22%3A%220036-8075%2C%201095-9203%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.sciencemag.org%5C%2Flookup%5C%2Fdoi%5C%2F10.1126%5C%2Fscience.123.3191.309%22%2C%22collections%22%3A%5B%225NYZ8VT6%22%5D%2C%22dateModified%22%3A%222020-03-19T15%3A53%3A30Z%22%7D%7D%2C%7B%22key%22%3A%22SIDRIKSV%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Van%20Wymelbeke%20et%20al.%22%2C%22parsedDate%22%3A%221998-08%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BVan%20Wymelbeke%20V%2C%20Himaya%20A%2C%20Louis-Sylvestre%20J%2C%20Fantino%20M%20%281998%29%20Influence%20of%20medium-chain%20and%20long-chain%20triacylglycerols%20on%20the%20control%20of%20food%20intake%20in%20men.%20Am%20J%20Clin%20Nutr%2068%3A226%26%23x2013%3B234.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Fajcn%5C%2F68.2.226%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Fajcn%5C%2F68.2.226%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Influence%20of%20medium-chain%20and%20long-chain%20triacylglycerols%20on%20the%20control%20of%20food%20intake%20in%20men%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22V.%22%2C%22lastName%22%3A%22Van%20Wymelbeke%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Himaya%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Louis-Sylvestre%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Fantino%22%7D%5D%2C%22abstractNote%22%3A%22Hunger%20may%20be%20delayed%20and%20food%20intake%20reduced%20under%20metabolic%20conditions%20that%20spare%20carbohydrate%20oxidation%2C%20especially%20during%20oxidation%20of%20medium-chain%20triacylglycerols%20%28MCTs%29%20or%20monounsaturated%20triacylglycerols.%20In%2012%20healthy%2C%20adult%2C%20male%20volunteers%20isolated%20and%20deprived%20of%20any%20time%20cues%2C%20we%20compared%20the%20effects%20of%204%20high-carbohydrate%20breakfasts%20%281670%20kJ%29%20supplemented%20either%20with%20a%20fat%20substitute%20%28Sub%3B%2070%20kJ%29%20or%20with%201460%20kJ%20fat%20as%20monounsaturated%20long-chain%20triacylglycerols%20%28LCT-U%29%2C%20saturated%20long-chain%20triacylglycerols%20%28LCT-S%29%2C%20or%20MCTs.%20In%20the%20first%20session%20we%20investigated%20the%20effects%20of%20these%20breakfasts%20on%20the%20following%20food%20intake%20variables%3A%20hunger%20ratings%20at%20repeated%20intervals%2C%20the%20time%20until%20the%20spontaneous%20request%20for%20the%20next%202%20free-choice%20meals%2C%20and%20the%20amount%20of%20food%20consumed.%20In%20a%20second%20session%20with%20fixed%20lunches%2C%20we%20studied%20the%20effects%20of%20the%20same%20breakfasts%20on%20plasma%20glucose%2C%20insulin%2C%20triacylglycerol%2C%20fatty%20acid%2C%20and%20beta-hydroxybutyrate%20concentrations.%20The%20addition%20of%20any%20of%20the%20fats%20to%20the%20high-carbohydrate%20breakfasts%20did%20not%20alter%20hunger%20ratings%2C%20but%20significantly%20delayed%20the%20request%20for%20lunch%20compared%20with%20the%20low-fat%20breakfast.%20The%20free-choice%20lunch%20eaten%20after%20the%20MCT%20breakfast%20was%20also%20significantly%20smaller.%20Blood%20glucose%20and%20insulin%20concentrations%20were%20lower%20after%20the%203%20fat%20breakfasts%2C%20followed%20by%20larger%20increases%20in%20glucose%20and%20enhanced%20insulin%20responses%2030%20min%20after%20the%20lunch.%20No%20differences%20were%20observed%20between%20the%20LCT-U%20and%20LCT-S%20conditions.%20We%20conclude%20that%20MCTs%20decreased%20food%20intake%20by%20a%20postabsorptive%20mechanism%2C%20although%20the%20exact%20effect%20of%20these%20lipids%20on%20carbohydrate%20oxidation%20will%20require%20further%20studies%20involving%20nutrient%20balance%20measurements.%22%2C%22date%22%3A%22Aug%201998%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1093%5C%2Fajcn%5C%2F68.2.226%22%2C%22ISSN%22%3A%220002-9165%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22HJKVZCPI%22%5D%2C%22dateModified%22%3A%222020-03-17T04%3A38%3A54Z%22%7D%7D%2C%7B%22key%22%3A%222KSJLCV8%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hellman%20et%20al.%22%2C%22parsedDate%22%3A%221969-11-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHellman%20DE%2C%20Senior%20B%2C%20Goodman%20HM%20%281969%29%20Anti-lipolytic%20effects%20of%20%26%23x3B2%3B-hydroxybutyrate.%20Metabolism%20-%20Clinical%20and%20Experimental%2018%3A906%26%23x2013%3B915.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2F0026-0495%2869%2990031-6%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2F0026-0495%2869%2990031-6%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anti-lipolytic%20effects%20of%20%5Cu03b2-hydroxybutyrate%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dorothea%20E.%22%2C%22lastName%22%3A%22Hellman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Boris%22%2C%22lastName%22%3A%22Senior%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22H.%20Maurice%22%2C%22lastName%22%3A%22Goodman%22%7D%5D%2C%22abstractNote%22%3A%22%26lt%3Bh2%26gt%3BAbstract%26lt%3B%5C%2Fh2%26gt%3B%26lt%3Bp%26gt%3BThe%20addition%20of%20%5Cu03b2-hydroxybutyrate%20to%20epididymal%20fat%20incubated%20in%20vitro%20reduced%20the%20production%20of%20glycerol%20and%20free%20fatty%20acids.%20Inhibition%20of%20lipolysis%20was%20maximal%20%28%5Cu223c%2030%25%29%20when%20physiologic%20concentrations%20of%20%5Cu03b2-hydroxybutyrate%20%280.1%20mg.%5C%2Fml.%29%20were%20added%20to%20tissues%20obtained%20from%20fasting%20rats.%20At%20a%20concentration%20of%2010%20mg.%5C%2Fml.%2C%20%5Cu03b2-hydroxybutyrate%20also%20abolished%20lipolysis%20in%20response%20to%200.05%20%5Cu03bcg.%5C%2Fml.%20epinephrine%20and%20severely%20reduced%20the%20lipolytic%20effects%20of%20ACTH%20%281%20%5Cu03bcg.%5C%2Fml.%29%2C%20TSH%20%2825%20mU%5C%2Fml.%29%20and%20glucagon%20%2810%20%5Cu03bcg.%5C%2Fml.%29.%20Increasing%20the%20concentration%20of%20epinephrine%20produced%20a%20progressive%20but%20significantly%20lesser%20lipolytic%20response%20in%20%5Cu03b2-hydroxybutyrate%20treated%20%2810%20mg.%5C%2Fml.%29%20than%20in%20control%20tissues.%20%5Cu03b2-hydroxybutyrate%2C%2010%20mg.%5C%2Fml.%2C%20abolished%20the%20lipolytic%20response%20to%20theophylline%20%280.54%20mg.%5C%2Fml.%29%2C%20but%20did%20not%20inhibit%20the%20lipolytic%20response%20to%20exogenous%20cyclic%20adenosine%203%5Cu2032%2C5%5Cu2032-monophosphate%20%28CAMP%29%20in%20the%20presence%20of%20theophylline.%20These%20results%20are%20consistent%20with%20the%20concept%20that%20%5Cu03b2-hydroxbutyrate%20may%20modulate%20the%20production%20of%20fatty%20acids%20during%20fasting%20and%20suggest%20that%20the%20antagonism%20of%20epinephrine-induced%20lipolysis%20may%20result%20from%20inhibition%20of%20CAMP%20formation%20in%20adipose%20tissue.%26lt%3B%5C%2Fp%26gt%3B%22%2C%22date%22%3A%221969%5C%2F11%5C%2F01%22%2C%22language%22%3A%22English%22%2C%22DOI%22%3A%2210.1016%5C%2F0026-0495%2869%2990031-6%22%2C%22ISSN%22%3A%220026-0495%2C%201532-8600%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.metabolismjournal.com%5C%2Farticle%5C%2F0026-0495%2869%2990031-6%5C%2Fabstract%22%2C%22collections%22%3A%5B%22TPPQF3UK%22%5D%2C%22dateModified%22%3A%222020-03-16T09%3A51%3A18Z%22%7D%7D%2C%7B%22key%22%3A%225JRYL8UX%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Newport%20et%20al.%22%2C%22parsedDate%22%3A%222015-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNewport%20MT%2C%20VanItallie%20TB%2C%20Kashiwaya%20Y%2C%20et%20al%20%282015%29%20A%20new%20way%20to%20produce%20hyperketonemia%3A%20use%20of%20ketone%20ester%20in%20a%20case%20of%20Alzheimer%26%23x2019%3Bs.%20Alzheimers%20Dement%2011%3A99%26%23x2013%3B103.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jalz.2014.01.006%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jalz.2014.01.006%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20new%20way%20to%20produce%20hyperketonemia%3A%20use%20of%20ketone%20ester%20in%20a%20case%20of%20Alzheimer%5Cu2019s%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mary%20T.%22%2C%22lastName%22%3A%22Newport%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Theodore%20B.%22%2C%22lastName%22%3A%22VanItallie%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoshihiro%22%2C%22lastName%22%3A%22Kashiwaya%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%20Todd%22%2C%22lastName%22%3A%22King%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20L.%22%2C%22lastName%22%3A%22Veech%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-1%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jalz.2014.01.006%22%2C%22ISSN%22%3A%221552-5260%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC4300286%5C%2F%22%2C%22collections%22%3A%5B%22TPPQF3UK%22%5D%2C%22dateModified%22%3A%222020-03-16T01%3A51%3A50Z%22%7D%7D%2C%7B%22key%22%3A%22QU6JIB96%22%2C%22library%22%3A%7B%22id%22%3A5748374%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Cavaleri%20and%20Bashar%22%2C%22parsedDate%22%3A%222018-04-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%20%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCavaleri%20F%2C%20Bashar%20E%20%282018%29%20Potential%20Synergies%20of%20%26%23x3B2%3B-Hydroxybutyrate%20and%20Butyrate%20on%20the%20Modulation%20of%20Metabolism%2C%20Inflammation%2C%20Cognition%2C%20and%20General%20Health.%20J%20Nutr%20Metab%202018%3A.%20%26lt%3Ba%20class%3D%26%23039%3Bzp-DOIURL%26%23039%3B%20href%3D%26%23039%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1155%5C%2F2018%5C%2F7195760%26%23039%3B%26gt%3Bhttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1155%5C%2F2018%5C%2F7195760%26lt%3B%5C%2Fa%26gt%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Potential%20Synergies%20of%20%5Cu03b2-Hydroxybutyrate%20and%20Butyrate%20on%20the%20Modulation%20of%20Metabolism%2C%20Inflammation%2C%20Cognition%2C%20and%20General%20Health%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Franco%22%2C%22lastName%22%3A%22Cavaleri%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Emran%22%2C%22lastName%22%3A%22Bashar%22%7D%5D%2C%22abstractNote%22%3A%22The%20low-carbohydrate%20high-fat%20diet%20%28LCHFD%29%2C%20also%20known%20as%20the%20ketogenic%20diet%2C%20has%20cycled%20in%20and%20out%20of%20popularity%20for%20decades%20as%20a%20therapeutic%20program%20to%20treat%20metabolic%20syndrome%2C%20weight%20mismanagement%2C%20and%20drug-resistant%20disorders%20as%20complex%20as%20epilepsy%2C%20cancer%2C%20dementia%2C%20and%20depression.%20Despite%20the%20benefits%20of%20this%20diet%2C%20health%20care%20professionals%20still%20question%20its%20safety%20due%20to%20the%20elevated%20serum%20ketones%20it%20induces%20and%20the%20limited%20dietary%20fiber.%20To%20compound%20the%20controversy%2C%20patient%20compliance%20with%20the%20program%20is%20poor%20due%20to%20the%20restrictive%20nature%20of%20the%20diet%20and%20symptoms%20related%20to%20energy%20deficit%20and%20gastrointestinal%20adversity%20during%20the%20introductory%20and%20energy%20substrate%20transition%20phase%20of%20the%20diet.%20The%20studies%20presented%20here%20demonstrate%20safety%20and%20efficacy%20of%20the%20diet%20including%20the%20scientific%20support%20and%20rationale%20for%20the%20administration%20of%20exogenous%20ketone%20bodies%20and%20ketone%20sources%20as%20a%20complement%20to%20the%20restrictive%20dietary%20protocol%20or%20as%20an%20alternative%20to%20the%20diet.%20This%20review%20also%20highlights%20the%20synergy%20provided%20by%20exogenous%20ketone%2C%20%5Cu03b2-hydroxybutyrate%20%28BHB%29%2C%20accompanied%20by%20the%20short%20chain%20fatty%20acid%2C%20butyrate%20%28BA%29%20in%20the%20context%20of%20cellular%20and%20physiological%20outcomes.%20More%20work%20is%20needed%20to%20unveil%20the%20molecular%20mechanisms%20by%20which%20this%20program%20provides%20health%20benefits.%22%2C%22date%22%3A%222018-4-1%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1155%5C%2F2018%5C%2F7195760%22%2C%22ISSN%22%3A%222090-0724%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC5902005%5C%2F%22%2C%22collections%22%3A%5B%22TPPQF3UK%22%5D%2C%22dateModified%22%3A%222020-03-16T01%3A37%3A17Z%22%7D%7D%5D%7D
1.
Dietze G, Wicklmayr M, Grunst J, Mehnert H (1976) [The anti-ketogenic effect of fructose]. Verh Dtsch Ges Inn Med 82 Pt 1:767–769
1.
Lee BM, Wolever TM (1998) Effect of glucose, sucrose and fructose on plasma glucose and insulin responses in normal humans: comparison with white bread. Eur J Clin Nutr 52:924–928.
https://doi.org/10.1038/sj.ejcn.1600666
1.
Pawlosky RJ, Kashiwaya Y, King MT, Veech RL (2020) A Dietary Ketone Ester Normalizes Abnormal Behavior in a Mouse Model of Alzheimer’s Disease. IJMS 21:1044.
https://doi.org/10.3390/ijms21031044
1.
Poulain M, Pes GM, Grasland C, et al (2004) Identification of a geographic area characterized by extreme longevity in the Sardinia island: the AKEA study. Experimental Gerontology 39:1423–1429.
https://doi.org/10.1016/j.exger.2004.06.016
1.
Esposito K, Chiodini P, Colao A, et al (2012) Metabolic Syndrome and Risk of Cancer: A systematic review and meta-analysis. Diabetes Care 35:2402–2411.
https://doi.org/10.2337/dc12-0336
1.
Seeman TE, Crimmins E, Huang M-H, et al (2004) Cumulative biological risk and socio-economic differences in mortality: MacArthur Studies of Successful Aging. Social Science & Medicine 58:1985–1997.
https://doi.org/10.1016/S0277-9536(03)00402-7
1.
Pinquart M, Sörensen S (2000) Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychology and Aging 15:187–224.
https://doi.org/10.1037/0882-7974.15.2.187
1.
Lemaître J-F, Ronget V, Tidière M, et al (2020) Sex differences in adult lifespan and aging rates of mortality across wild mammals. Proc Natl Acad Sci USA.
https://doi.org/10.1073/pnas.1911999117
1.
Madsen EL, Rissanen A, Bruun JM, et al (2008) Weight loss larger than 10% is needed for general improvement of levels of circulating adiponectin and markers of inflammation in obese subjects: a 3-year weight loss study. European Journal of Endocrinology 158:179–187.
https://doi.org/10.1530/EJE-07-0721
1.
Nguyen NT, Nguyen X-MT, Wooldridge JB, et al (2010) Association of obesity with risk of coronary heart disease: findings from the National Health and Nutrition Examination Survey, 1999–2006. Surgery for Obesity and Related Diseases 6:465–469.
https://doi.org/10.1016/j.soard.2010.02.038
1.
Partsalaki I, Karvela A, Spiliotis BE (2012) Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J Pediatr Endocrinol Metab 25:697–704.
https://doi.org/10.1515/jpem-2012-0131
1.
Kosinski C, Jornayvaz F (2017) Effects of Ketogenic Diets on Cardiovascular Risk Factors: Evidence from Animal and Human Studies. Nutrients 9:517.
https://doi.org/10.3390/nu9050517
1.
Włodarek D (2019) Role of Ketogenic Diets in Neurodegenerative Diseases (Alzheimer’s Disease and Parkinson’s Disease). Nutrients 11:169.
https://doi.org/10.3390/nu11010169
1.
Fine E Targeting insulin inhibition as a metabolic therapy in advanced cancer: a pilot safety and feasibility dietary trial in 10 patients. - PubMed - NCBI.
https://www.ncbi.nlm.nih.gov/pubmed/22840388. Accessed 19 Mar 2020
1.
Kentaro Nakamura, Hidekazu Tonouchi, Akina Sasayama, Kinya Ashida (2018) A Ketogenic Formula Prevents Tumor Progression and Cancer Cachexia by Attenuating Systemic Inflammation in Colon 26 Tumor-Bearing Mice. Nutrients 10:206.
https://doi.org/10.3390/nu10020206
1.
Lv M, Zhu X, Wang H, et al (2014) Roles of Caloric Restriction, Ketogenic Diet and Intermittent Fasting during Initiation, Progression and Metastasis of Cancer in Animal Models: A Systematic Review and Meta-Analysis. PLoS ONE 9:e115147.
https://doi.org/10.1371/journal.pone.0115147
1.
Poff AM, Ari C, Seyfried TN, D’Agostino DP (2013) The Ketogenic Diet and Hyperbaric Oxygen Therapy Prolong Survival in Mice with Systemic Metastatic Cancer. PLoS ONE 8:e65522.
https://doi.org/10.1371/journal.pone.0065522
1.
Van Wymelbeke V, Himaya A, Louis-Sylvestre J, Fantino M (1998) Influence of medium-chain and long-chain triacylglycerols on the control of food intake in men. Am J Clin Nutr 68:226–234.
https://doi.org/10.1093/ajcn/68.2.226
1.
Cavaleri F, Bashar E (2018) Potential Synergies of β-Hydroxybutyrate and Butyrate on the Modulation of Metabolism, Inflammation, Cognition, and General Health. J Nutr Metab 2018:.
https://doi.org/10.1155/2018/7195760