ONE Actionable Takeaway from Ketosource
One of the top complaints we get about fasting is trouble with sleep. This is largely due to the promotion of sleep-disturbing hormones.
The most effective way to solve this is a four-step process.
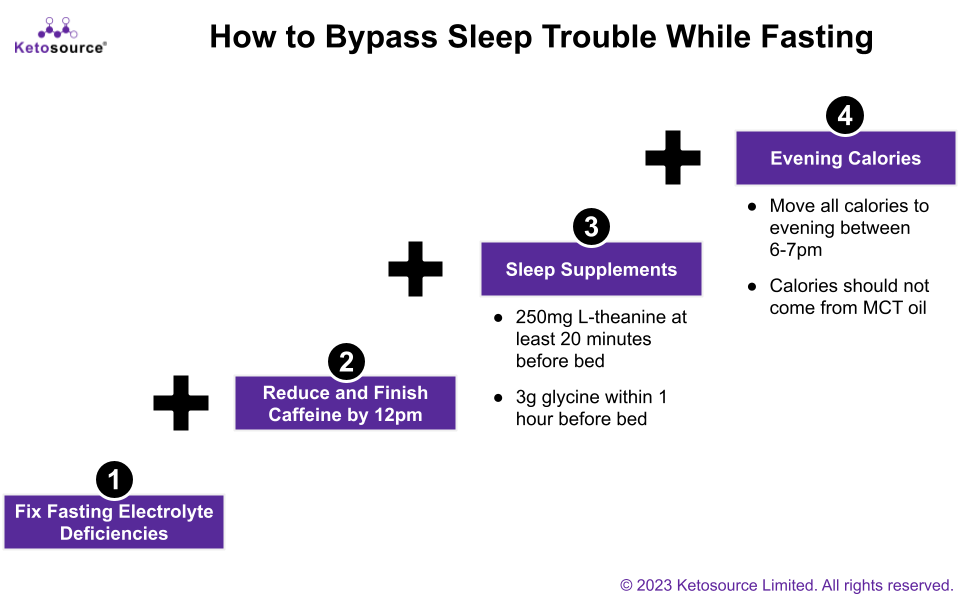
Start with just the first step. You only need to take extra steps, one by one, should the problem persist. Most people won’t need to do all four.
- Electrolytes: Use our electrolyte calculator to solve deficiencies.
- Caffeine: Finish all caffeine intake by 12pm and reduce your daily intake if you still feel alert by bedtime.
- Sleep Supplements: Take l-theanine and glycine before bedtime as they help with sleep.
- Evening calories: Move all or some of the calories you eat on your fasting days to the evening between 6 and 7 pm (e.g. your one meal of the day). But don’t take MCT oil in the evening as it can promote sleep issues for some people.
Research References
- The hormones epinephrine and norepinephrine (reviewed in ) are involved in waking/ wakefulness
- Reducing blood sugar is associated with the release of epinephrine and norepinephrine
- Reduced sodium intake is associated with increased epinephrine and norepinephrine
- Magnesium deficiency is associated with increased epinephrine and norepinephrine in rats
- Caffeine promotes wakefulness (reviewed in )
- Theanine improves sleep quality at doses as low as 250mg
- Theanine may take effect as soon as 15 minutes after taking it, though it can take longer to reach peak plasma levels
- Taking 3g of glycine within one hour before bed can improve various aspects of sleep quality
- We do not have evidence from the literature relating sleep to eating calories before bed. But foods may promote sleep via mechanisms tied to blood sugar and electrolytes as outlined here. So we suspect that eating some calories before sleep may promote sleep as well.
- Anecdotal evidence from clients suggests that MCT oils may disrupt sleep when taken too close to bedtime. Though we don’t know the exact mechanism for this, we suspect that it involves the metabolism of MCT oils. Based on the ketogenic response to MCT oils (plus buffer time), we recommend keeping at least 4 hours between your last dose of MCT and bedtime.
ONE Quote from a Credible Expert
How the ketogenic diet impacted military personnel from Dr. Jeff Volek. Jeff is a professor researching ketogenic diets in the Department of Human Sciences at Ohio State University. He’s also a founder of Virta Health, the company successfully reversing type 2 diabetes via ketogenic diets:
“The results [of our study on military personnel] were quite extraordinary… the protocol, that we use in, in studies, we don’t prescribe calories in a lot of these free living studies. So, we really enforce the low-carb piece of it and monitor ketones, but we allow people to eat, as, until, they’re full.
So, “eat to satiety” is what we say. So, there was no recommendation to restrict calories.
Yet, every single participant lost weight. And we measured body composition by, you know, arguably the gold standard, DEXA, and they were, able to demonstrate remarkable improvement in body composition as well. So, they’re actually, you know, maintaining most of their lean mass while losing a lot of fat mass.”
Source: Ketogenic Diet to improve metabolic health and treat disease | STEM Talk Episode 149 | 23 February 2023 (timestamp:
00:43:35)
Research References
- The research study that Dr. Volek is referencing
ONE of Your #1 Questions Answered
The Question:
The top question sent in from you this week was from Rami Khateeb. Thank you Rami!
“What are your thoughts on Exogenous Ketones supplements if someone is taking them without following a ketogenic diet? And what is your opinion of different brands like the one from Pruvit company (keto//os)?”
The Answer:
Exogenous Ketones without a Ketogenic Diet
Exogenous ketone supplements will increase your ketone level regardless of your diet. Research I’ve read supports this as well as internal experiments we ran at Ketosource.
So if you prefer not to follow a ketogenic diet, you can still expect a ketone boost from exogenous ketones.
Evaluating Specific Exogenous Ketone Supplements
There are four types of exogenous ketone supplements: ketone salts, ketone esters, MCT oils and 1,3 Butanediol.
We have run experiments to test the peak ketone boost per serving of several of these supplements. We then also benchmarked the cost per serving for each supplement. The chart below illustrates this analysis.
As you can see, there is a wide range of prices per serving and peak ketone boost for exogenous ketone supplements.

The Takeaway
- Aim for your minimum effective ketone boost. More is not necessarily better. The ketone boost you should aim for depends on your goal. For fat loss, appetite reduction ketosis is all you need (0.5 mmol/L). For other goals, it can be higher.
- Get the most value by comparing exogenous ketone supplements on a cost per serving basis. Compare exogenous ketone supplements that meet your ketone boost needs on a cost per serving basis. That way you can meet your goal at the lowest cost.
Research References
- Exogenous ketone experiment data: Ketosource analysis, Ketosource N=2 experiment data sets. Public recommended retail price (RRP) used.
- Note that the specific supplement formulations and their behavior may have changed since this experiment. Yet, the general comparison between ketone esters vs. ketone salts vs. C8 MCT will hold true. Read the full details on the experiment here.
- Ketone salts, ketone esters, MCT oils, and 1,3-butanediol can all boost ketone levels.
KET-ONE Sunday?
Just hit reply to this email and ask your question.
Continuous Ketone Monitor Experiment – What You Decided to Test
I’m guinea-pigging myself in a continuous ketone monitor self-experiment.
I crowd sourced what the experiment should be last week with you. And here’s what you voted on.

Next steps? We will design the 14-day experiment to include your four top-voted experiments (the black segments from the chart above).
Then it will be guinea-pig time. A big thanks to everyone who voted on ‘one night of poor sleep’ by the way – the things I do for citizen science!
I’ll update you in future editions of KET-ONE Sunday as this unfolds.